Abstract
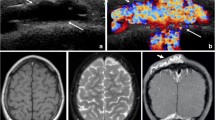
Vascular anomalies, further classified into vascular tumors and malformations, often involve the head and neck region of children. These entities may raise diagnostic dilemmas, as they often demonstrate heterogenous and overlapping histologic features. The aim of this paper is to provide an overview of the common vascular anomalies in the head and neck region of children. Specific entities discussed include infantile hemangioma, congenital hemangioma, tufted angioma, kaposiform hemangioendothelioma, and various vascular malformations. Clinicopathologic features and associated molecular associations are reviewed.




Similar content being viewed by others
References
Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412–22.
Munden A, Butschek R, Tom WL, Marshall JS, Poeltler DM, Krohne SE, et al. Prospective study of infantile haemangiomas: incidence, clinical characteristics and association with placental anomalies. Br J Dermatol. 2014;170:907–13.
O’Brien KF, Shah SD, Pope E, Phillips RJ, Blei F, Baselga E, et al. Late growth of infantile hemangiomas in children >3 years of age: a retrospective study. J Am Acad Dermatol. 2019;80:493–9.
Krowchuk DP, Frieden IJ, Mancini AJ, Darrow DH, Blei F, Greene AK, et al. Clinical practice guideline for the management of infantile hemangiomas. Pediatrics. 2019;143:e20183475.
Jinnin M, Medici D, Park L, Limaye N, Liu Y, Boscolo E, et al. Suppressed NFAT-dependent VEGFR1 expression and constitutive VEGFR2 signaling in infantile hemangioma. Nat Med. 2008;14:1236–46.
Boye E, Olsen BR. Signaling mechanisms in infantile hemangioma. Curr Opin Hematol. 2009;16:202–8.
Iyer NV, Kotch LE, Agani F, Leung SW, Laughner E, Wenger RH, et al. Cellular and developmental control of O2 homeostasis by hypoxia-inducible factor 1 alpha. Genes Dev. 1998;12:149–62.
North PE. Pediatric vascular tumors and malformations. Surg Pathol Clin. 2010;3:455–94.
Brahmbhatt AN, Skalski KA, Bhatt AA. Vascular lesions of the head and neck: an update on classification and imaging review. Insights Imaging. 2020;11:19.
North PE, Waner M, Mizeracki A, Mihm MC. GLUT1: a newly discovered immunohistochemical marker for juvenile hemangiomas. Hum Pathol. 2000;31:11–22.
Gupta A, Kozakewich H. Histopathology of vascular anomalies. Clin Plast Surg. 2011;38:31–44.
Jeng MR, Fuh B, Blatt J, Gupta A, Merrow AC, Hammill A, et al. Malignant transformation of infantile hemangioma to angiosarcoma: response to chemotherapy with bevacizumab. Pediatr Blood Cancer. 2014;61:2115–7.
Kanada KN, Merin MR, Munden A, Friedlander SF. A prospective study of cutaneous findings in newborns in the United States: correlation with race, ethnicity, and gestational status using updated classification and nomenclature. J Pediatr. 2012;161:240–5.
Bruder E, Alaggio R, Kozakewich HPW, Jundt G, Dehner LP, Coffin CM. Vascular and perivascular lesions of skin and soft tissues in children and adolescents. Pediatr Dev Pathol. 2012;15:26–61.
Berenguer B, Mulliken JB, Enjolras O, Boon LM, Wassef M, Josset P, et al. Rapidly involuting congenital hemangioma: clinical and histopathologic features. Pediatr Dev Pathol. 2003;6:495–510.
Blumenthal S, Stefanko N, Cossio M-L, Coulombe J, McCuaig C, Dubois J, et al. Multifocal congenital hemangioma: expanding the pathogenesis of “neonatal hemangiomatosis.” Pediatr Dermatol. 2019;36:720–2.
Baselga E, Cordisco MR, Garzon M, Lee MT, Alomar A, Blei F. Rapidly involuting congenital haemangioma associated with transient thrombocytopenia and coagulopathy: a case series. Br J Dermatol. 2008;158:1363–70.
Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, et al. Vascular anomalies classification: recommendations from the International Society for the Study of Vascular Anomalies. Pediatrics. 2015;136:e203-214.
Maguiness S, Uihlein LC, Liang MG, Kozakewich H, Mulliken JB. Rapidly involuting congenital hemangioma with fetal involution. Pediatr Dermatol. 2015;32:321–6.
Ayturk UM, Couto JA, Hann S, Mulliken JB, Williams KL, Huang AY, et al. Somatic activating mutations in GNAQ and GNA11 are associated with congenital hemangioma. Am J Hum Genet. 2016;98:1271.
Merrow AC, Gupta A, Patel MN, Adams DM. 2014 Revised classification of vascular lesions from the International Society for the Study of Vascular Anomalies: radiologic-pathologic update. Radiographics. 2016;36:1494–516.
Vildy S, Macher J, Abasq-Thomas C, Le Rouzic-Dartoy C, Brunelle F, Hamel-Teillac D, et al. Life-threatening hemorrhaging in neonatal ulcerated congenital hemangioma: two case reports. JAMA Dermatol. 2015;151:422–5.
Osio A, Fraitag S, Hadj-Rabia S, Bodemer C, de Prost Y, Hamel-Teillac D. Clinical spectrum of tufted angiomas in childhood: a report of 13 cases and a review of the literature. Arch Dermatol. 2010;146:758–63.
Feito-Rodríguez M, Sánchez-Orta A, De Lucas R, López-Gutiérrez JC, Ruiz-Bravo E, Baselga E, et al. Congenital tufted angioma: a multicenter retrospective study of 30 cases. Pediatr Dermatol. 2018;35:808–16.
Häußler SM, Uecker FC, Knopke S, Roßner F, Olze H, Böttcher A. Tufted angiomas of the head and neck. HNO. 2018;66:1–6.
Herron MD, Coffin CM, Vanderhooft SL. Tufted angiomas: variability of the clinical morphology. Pediatr Dermatol. 2002;19:394–401.
Mahajan P, Margolin J, Iacobas I. Kasabach-Merritt phenomenon: classic presentation and management options. Clin Med Insights Blood Disord. 2017. https://doi.org/10.1177/1179545X17699849.
Le Huu AR, Jokinen CH, Rubin BP, Ruben BP, Mihm MC, Weiss SW, et al. Expression of prox1, lymphatic endothelial nuclear transcription factor, in kaposiform hemangioendothelioma and tufted angioma. Am J Surg Pathol. 2010;34:1563–73.
Croteau SE, Gupta D. The clinical spectrum of kaposiform hemangioendothelioma and tufted angioma. Semin Cutan Med Surg. 2016;35:147–52.
Liu XH, Li JY, Qu XH, Yan WL, Zhang L, Yang C, et al. Treatment of kaposiform hemangioendothelioma and tufted angioma. Int J Cancer. 2016;139:1658–66.
Tasani M, Ancliff P, Glover M. Sirolimus therapy for children with problematic kaposiform haemangioendothelioma and tufted angioma. Br J Dermatol. 2017;177:e344–6.
Burleigh A, Kanigsberg N, Lam JM. Topical rapamycin (sirolimus) for the treatment of uncomplicated tufted angiomas in two children and review of the literature. Pediatr Dermatol. 2018;35:e286–90.
Croteau SE, Liang MG, Kozakewich HP, Alomari AI, Fishman SJ, Mulliken JB, et al. Kaposiform hemangioendothelioma: atypical features and risks of Kasabach-Merritt phenomenon in 107 referrals. J Pediatr. 2013;162:142–7.
Putra J, Gupta A. Kaposiform haemangioendothelioma: a review with emphasis on histological differential diagnosis. Pathology. 2017;49:356–62.
Wong BLK, Lee VNY, Tikka T, Kim D, Dwivedi RC. Kaposiform haemangioendothelioma of the head and neck. Crit Rev Oncol Hematol. 2016;104:156–68.
Enjolras O, Mulliken JB, Boon LM, Wassef M, Kozakewich HP, Burrows PE. Noninvoluting congenital hemangioma: a rare cutaneous vascular anomaly. Plast Reconstr Surg. 2001;107:1647–54.
Méndez R, Capdevila A, Tellado MG, Somoza I, Liras J, Pais E, et al. Kaposiform hemangioendothelioma associated with Milroy’s disease (primary hereditary lymphedema). J Pediatr Surg. 2003;38:E9-12.
Calvo-Garcia MA, Kline-Fath BM, Adams DM, Gupta A, Koch BL, Lim F-Y, et al. Imaging evaluation of fetal vascular anomalies. Pediatr Radiol. 2015;45:1218–29.
Mac-Moune Lai F, To KF, Choi PC, Leung PC, Kumta SM, Yuen PP, et al. Kaposiform hemangioendothelioma: five patients with cutaneous lesion and long follow-up. Mod Pathol. 2001;14:1087–92.
Adams DM, Trenor CC, Hammill AM, Vinks AA, Patel MN, Chaudry G, et al. Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics. 2016;137:e20153257.
Lyons LL, North PE, Mac-Moune Lai F, Stoler MH, Folpe AL, Weiss SW. Kaposiform hemangioendothelioma: a study of 33 cases emphasizing its pathologic, immunophenotypic, and biologic uniqueness from juvenile hemangioma. Am J Surg Pathol. 2004;28:559–68.
Hauer J, Graubner U, Konstantopoulos N, Schmidt S, Pfluger T, Schmid I. Effective treatment of kaposiform hemangioendotheliomas associated with Kasabach-Merritt phenomenon using four-drug regimen. Pediatr Blood Cancer. 2007;49:852–4.
Nguyen V, Hochman M, Mihm MC, Nelson JS, Tan W. The pathogenesis of port wine stain and Sturge Weber syndrome: complex interactions between genetic alterations and aberrant MAPK and PI3K activation. Int J Mol Sci. 2019;20:2243.
Lee JW, Chung HY. Vascular anomalies of the head and neck: current overview. Arch Craniofac Surg. 2018;19:243–7.
Mahady K, Thust S, Berkeley R, Stuart S, Barnacle A, Robertson F, et al. Vascular anomalies of the head and neck in children. Quant Imaging Med Surg. 2015;5:886–97.
Limaye N, Wouters V, Uebelhoer M, Tuominen M, Wirkkala R, Mulliken JB, et al. Somatic mutations in angiopoietin receptor gene TEK cause solitary and multiple sporadic venous malformations. Nat Genet. 2009;41:118–24.
Castel P, Carmona FJ, Grego-Bessa J, Berger MF, Viale A, Anderson KV, et al. Somatic PIK3CA mutations as a driver of sporadic venous malformations. Sci Transl Med. 2016;8:332ra42.
Luks VL, Kamitaki N, Vivero MP, Uller W, Rab R, Bovée JVMG, et al. Lymphatic and other vascular malformative/overgrowth disorders are caused by somatic mutations in PIK3CA. J Pediatr. 2015;166:1048-1054.e1-5.
Couto JA, Huang AY, Konczyk DJ, Goss JA, Fishman SJ, Mulliken JB, et al. Somatic MAP2K1 mutations are associated with extracranial arteriovenous malformation. Am J Hum Genet. 2017;100:546–54.
Fereydooni A, Dardik A, Nassiri N. Molecular changes associated with vascular malformations. J Vasc Surg. 2019;70(314–326):e1.
Funding
No funding obtained.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Research Involving Human and/or Animal Participants
This article does not contain any studies with human participants or animals performed by any of the author.
Consent for Publication
The participant has given consent to the submission of the case report to the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Putra, J., Al-Ibraheemi, A. Vascular Anomalies of the Head and Neck: A Pediatric Overview. Head and Neck Pathol 15, 59–70 (2021). https://doi.org/10.1007/s12105-020-01236-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-020-01236-x