Abstract
Purpose of Review
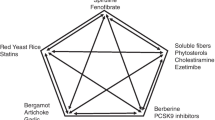
The aim of this review is to provide an update on the effects of the dietary supplementation with cholesterol-lowering nutraceuticals and nutraceutical combinations affecting vascular function and CV risk in clinical interventional studies.
Recent Findings
Current evidence supports the mild-to-moderate cholesterol-lowering efficacy of red yeast rice, berberine, plant sterols, fibers, and some nutraceutical combinations whereas data on the individual cholesterol-lowering action of other nutraceuticals are either less striking or even inconclusive. There is also promising evidence on the vascular protective effects of some of the aforementioned nutraceuticals. However, except for red yeast rice, clinical interventional studies have not investigated their impact on CV outcomes.
Summary
Evidence of both cholesterol-lowering and vascular protection is a prerogative of few single nutraceuticals and nutraceutical combinations, which may support their clinical use; however, caution on their uncontrolled adoption is necessary as they are freely available on the market and, therefore, subject to potential misuse.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25.
•• Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316:1289–97. In this meta-analysis, statin and non-statin therapy-reducing LDL cholesterol levels by upregulating LDL receptor were associated with a similar reduction of CV events per change in LDL cholesterol.
Alissa EM, Ferns GA. Functional foods and nutraceuticals in the primary prevention of cardiovascular diseases. J Nutr Metab. 2012;2012:569486.
Mannarino MR, Ministrini S, Pirro M. Nutraceuticals for the treatment of hypercholesterolemia. Eur J Intern Med. 2014;25:592–9.
Sahebkar A, Serban MC, Gluba-Brzózka A, Mikhailidis DP, Cicero AF, Rysz J, et al. Lipid-modifying effects of nutraceuticals: an evidence-based approach. Nutrition. 2016;32:1179–92.
Cicero AFG, Colletti A, Bajraktari G, Descamps O, Djuric DM, Ezhov M, et al. Lipid-lowering nutraceuticals in clinical practice: position paper from an International Lipid Expert Panel. Nutr Rev. 2017;75:731–67.
Pirro M, Vetrani C, Bianchi C, Mannarino MR, Bernini F, Rivellese AA. Joint position statement on “Nutraceuticals for the treatment of hypercholesterolemia” of the Italian Society of Diabetology (SID) and of the Italian Society for the Study of Arteriosclerosis (SISA). Nutr Metab Cardiovasc Dis. 2017;27:2–17.
Ward N, Sahebkar A, Banach M, Watts G. Recent perspectives on the role of nutraceuticals as cholesterol-lowering agents. Curr Opin Lipidol. 2017;28:495–501.
Johnston TP, Korolenko TA, Pirro M, Sahebkar A. Preventing cardiovascular heart disease: promising nutraceutical and non-nutraceutical treatments for cholesterol management. Pharmacol Res. 2017;120:219–25.
Viuda-Martos M, López-Marcos MC, Fernández-López J, Sendra E, López-Vargas J, Pérez-Álvarez J. Role of fiber in cardiovascular diseases: a review. Compr Rev Food Sci Food Saf. 2010;9:240–58.
Chutkan R, Fahey G, Wright WL, McRorie J. Viscous versus nonviscous soluble fiber supplements: mechanisms and evidence for fiber-specific health benefits. J Am Acad Nurse Pract. 2012;24:476–87.
Estruch R, Martínez-González MA, Corella D, Basora-Gallisá J, Ruiz-Gutiérrez V, Covas MI, et al. Effects of dietary fibre intake on risk factors for cardiovascular disease in subjects at high risk. J Epidemiol Community Health. 2009;63:582–8.
•• Ho HVT, Jovanovski E, Zurbau A, Blanco Mejia S, Sievenpiper JL, Au-Yeung F, et al. A systematic review and meta-analysis of randomized controlled trials of the effect of konjac glucomannan, a viscous soluble fiber, on LDL cholesterol and the new lipid targets non-HDL cholesterol and apolipoprotein B. Am J Clin Nutr. 2017;105:1239–47. This meta-analysis of 12 randomized clinical trials showed that the oral supplementation of konjac glucomannan reduced significantly LDL and non-HDL cholesterol, supporting its use at the daily dose of 3 g to achieve a reduction in LDL cholesterol and non-HDL cholesterol of 10 and 7%, respectively.
•• Ho HV, Sievenpiper JL, Zurbau A, Blanco Mejia S, Jovanovski E, Au-Yeung F, et al. A systematic review and meta-analysis of randomized controlled trials of the effect of barley β-glucan on LDL-C, non-HDL-C and apoB for cardiovascular disease risk reductioni-iv. Eur J Clin Nutr. 2016;70:1239–45. In this meta-analysis of 14 randomized clinical trials, oral supplementation of barley β-glucan at a mean daily dose of 6.5 and 6.9 g reduced significantly LDL cholesterol and non-HDL cholesterol levels.
Brown L, Rosner B, Willett WW, Sacks FM. Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr. 1999;69:30–42.
Sood N, Baker WL, Coleman CI. Effect of glucomannan on plasma lipid and glucose concentrations, body weight, and blood pressure: systematic review and meta-analysis. Am J Clin Nutr. 2008;88:1167–75.
Whitehead A, Beck EJ, Tosh S, Wolever TM. Cholesterol-lowering effects of oat β-glucan: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100:1413–21.
• Gulati S, Misra A, Pandey RM. Effects of 3 g of soluble fiber from oats on lipid levels of Asian Indians—a randomized controlled, parallel arm study. Lipids Health Dis. 2017;16:71. In this short-term, prospective, open-labeled, randomized, controlled parallel group study, 3 g of soluble fiber from 70 g of oats reduced significantly LDL cholesterol levels.
Reppas C, Swidan SZ, Tobey SW, Turowski M, Dressman JB. Hydroxypropylmethylcellulose significantly lowers blood cholesterol in mildly hypercholesterolemic human subjects. Eur J Clin Nutr. 2009;63:71–7.
•• Evans CE, Greenwood DC, Threapleton DE, Cleghorn CL, Nykjaer C, Woodhead CE, et al. Effects of dietary fibre type on blood pressure: a systematic review and meta-analysis of randomized controlled trials of healthy individuals. J Hypertens. 2015;33:897–911. In this meta-analysis of 18 randomized controlled trials, a high dietary consumption of beta-glucan reduced significantly blood pressure levels.
Breneman CB, Tucker L. Dietary fibre consumption and insulin resistance—the role of body fat and physical activity. Br J Nutr. 2013;110:375–83.
Ma Y, Hébert JR, Li W, Bertone-Johnson ER, Olendzki B, Pagoto SL, et al. Association between dietary fiber and markers of systemic inflammation in the Women’s Health Initiative Observational Study. Nutrition. 2008;24:941–9.
Marckmann P, Sandström B, Jespersen J. Low-fat, high-fiber diet favorably affects several independent risk markers of ischemic heart disease: observations on blood lipids, coagulation, and fibrinolysis from a trial of middle-aged Danes. Am J Clin Nutr. 1994;59:935–9.
• Kondo K, Morino K, Nishio Y, Ishikado A, Arima H, Nakao K, et al. Fiber-rich diet with brown rice improves endothelial function in type 2 diabetes mellitus: a randomized controlled trial. PLoS One. 2017;12:e0179869. In this randomized clinical trial, a fiber-enriched diet containing brown rice 5.6 g/day improved significantly endothelial function compared to a fiber-enriched diet containing white rice 1.2 g/day.
• Cosola C, De Angelis M, Rocchetti MT, Montemurno E, Maranzano V, Dalfino G, et al. Beta-glucans supplementation associates with reduction in P-cresyl sulfate levels and improved endothelial vascular reactivity in healthy individuals. PLoS One. 2017;12:e0169635. This interventional study showed that the daily administration of pasta enriched with barley beta-glucans (3 g/100 g) improved significantly endothelial reactivity in 26 healthy volunteers.
Tabesh F, Sanei H, Jahangiri M, Momenizadeh A, Tabesh E, Pourmohammadi K, et al. The effects of beta-glucan rich oat bread on serum nitric oxide and vascular endothelial function in patients with hypercholesterolemia. Biomed Res Int. 2014;2014:481904.
Momenizadeh A, Heidari R, Sadeghi M, Tabesh F, Ekramzadeh M, Haghighatian Z, et al. Effects of oat and wheat bread consumption on lipid profile, blood sugar, and endothelial function in hypercholesterolemic patients: a randomized controlled clinical trial. ARYA Atheroscler. 2014;10:259–65.
Thazhath SS, Wu T, Bound MJ, Checklin HL, Jones KL, Willoughby S, et al. Changes in meal composition and duration affect postprandial endothelial function in healthy humans. Am J Physiol Gastrointest Liver Physiol. 2014;307:G1191–7.
Pal S, Khossousi A, Binns C, Dhaliwal S, Radavelli-Bagatini S. The effects of 12-week psyllium fibre supplementation or healthy diet on blood pressure and arterial stiffness in overweight and obese individuals. Br J Nutr. 2012;107:725–34.
Yoshida M, Sawa J, Hozumi T, Mimoto H, Ishida Y, Kazumi T, et al. Effects of long-term high-fiber diet on macrovascular changes and lipid and glucose levels in STZ-induced diabetic SD rats. Diabetes Res Clin Pract. 1991;13:147–52.
• Aoki S, KojiKawata A, Muramatsu D, Uchiyama H, Okabe M, Ikesue M, et al. Oral administration of the β-glucan produced by Aureobasidium pullulans ameliorates development of atherosclerosis in apolipoprotein E deficient mice. J Funct Foods. 2015;18:22–7. In apolipoprotein E-deficient mice, the oral administration of Aureobasidium pullulans -produced β-glucan reduced blood levels of oxidized LDL cholesterol and vascular accumulation of macrophages.
Wu H, Dwyer KM, Fan Z, Shircore A, Fan J, Dwyer JH. Dietary fiber and progression of atherosclerosis: the Los Angeles Atherosclerosis Study. Am J Clin Nutr. 2003;78:1085–91.
Cerda JJ, Normann SJ, Sullivan MP, Burgin CW, Robbins FL, Vathada S, et al. Inhibition of atherosclerosis by dietary pectin in microswine with sustained hypercholesterolemia. Circulation. 1994;89:1247–53.
Moreno Franco B, León Latre M, Andrés Esteban EM, Ordovás JM, Casasnovas JA, Peñalvo JL. Soluble and insoluble dietary fibre intake and risk factors for metabolic syndrome and cardiovascular disease in middle-aged adults: the AWHS cohort. Nutr Hosp. 2014;30:1279–88.
• Lu L, Huang YF, Wang MQ, Chen DX, Wan H, Wei LB, et al. Dietary fiber intake is associated with chronic kidney disease (CKD) progression and cardiovascular risk, but not protein nutritional status, in adults with CKD. Asia Pac J Clin Nutr. 2017;26:598–605. In this prospective observational study, a high dietary fiber intake (>25g/day) was associated with a significant reduction of inflammation parameters and cardiovascular risk in patients with chronic kidney disease.
• Buil-Cosiales P, Martinez-Gonzalez MA, Ruiz-Canela M, Díez-Espino J, García-Arellano A, Toledo E. Consumption of fruit or fiber-fruit decreases the risk of cardiovascular disease in a Mediterranean young cohort. Nutrients. 2017;9:295. In this observational prospective study, an inverse association between fiber intake and CV disease events was observed in a Mediterranean cohort of young adults.
Erkkilä AT, Lichtenstein AH. Fiber and cardiovascular disease risk: how strong is the evidence? J Cardiovasc Nurs. 2006;21:3–8.
McRae MP. Dietary fiber is beneficial for the prevention of cardiovascular disease: an umbrella review of meta-analyses. J Chiropr Med. 2017;16:289–99.
Threapleton DE, Greenwood DC, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2013;347:f6879.
Gylling H, Simonen P. Are plant sterols and plant stanols a viable future treatment for dyslipidemia? Expert Rev Cardiovasc Ther. 2016;14:549–51.
Andersson SW, Skinner J, Ellegård L, Welch AA, Bingham S, Mulligan A, et al. Intake of dietary plant sterols is inversely related to serum cholesterol concentration in men and women in the EPIC Norfolk population: a cross-sectional study. Eur J Clin Nutr. 2004;58:1378–85.
Mannarino E, Pirro M, Cortese C, Lupattelli G, Siepi D, Mezzetti A, et al. Effects of a phytosterol-enriched dairy product on lipids, sterols and 8-isoprostane in hypercholesterolemic patients: a multicenter Italian study. Nutr Metab Cardiovasc Dis. 2009;19:84–90.
Wu T, Fu J, Yang Y, Zhang L, Han J. The effects of phytosterols/stanols on blood lipid profiles: a systematic review with meta-analysis. Asia Pac J Clin Nutr. 2009;18:179–86.
Athyros VG, Kakafika AI, Papageorgiou AA, Tziomalos K, Peletidou A, Vosikis C, et al. Effect of a plant stanol ester-containing spread, placebo spread, or Mediterranean diet on estimated cardiovascular risk and lipid, inflammatory and haemostatic factors. Nutr Metab Cardiovasc Dis. 2011;21:213–21.
Othman RA, Moghadasian MH. Beyond cholesterol-lowering effects of plant sterols: clinical and experimental evidence of anti-inflammatory properties. Nutr Rev. 2011;69:371–82.
• Ras RT, Fuchs D, Koppenol WP, Garczarek U, Greyling A, Keicher C, et al. The effect of a low-fat spread with added plant sterols on vascular function markers: results of the Investigating Vascular Function Effects of Plant Sterols (INVEST) study. Am J Clin Nutr. 2015;101:733–41. In this double-blind, randomized, placebo-controlled study, the oral intake of a low-fat spread with added plant sterols did not improve endothelial function in hypercholesterolemic patients.
Gylling H, Halonen J, Lindholm H, Konttinen J, Simonen P, Nissinen MJ, et al. The effects of plant stanol ester consumption on arterial stiffness and endothelial function in adults: a randomised controlled clinical trial. BMC Cardiovasc Disord. 2013;13:50.
Hallikainen M, Lyyra-Laitinen T, Laitinen T, Agren JJ, Pihlajamäki J, Rauramaa R, et al. Endothelial function in hypercholesterolemic subjects: effects of plant stanol and sterol esters. Atherosclerosis. 2006;188:425–32.
Kelly ER, Plat J, Mensink RP, Berendschot TT. Effects of long term plant sterol and -stanol consumption on the retinal vasculature: a randomized controlled trial in statin users. Atherosclerosis. 2011;214:225–30.
de Jongh S, Vissers MN, Rol P, Bakker HD, Kastelein JJ, Stroes ES. Plant sterols lower LDL cholesterol without improving endothelial function in prepubertal children with familial hypercholesterolaemia. J Inherit Metab Dis. 2003;26:343–51.
Horenstein RB, Mitchell BD, Post WS, Lütjohann D, von Bergmann K, Ryan KA, et al. The ABCG8 G574R variant, serum plant sterol levels, and cardiovascular disease risk in the Old Order Amish. Arterioscler Thromb Vasc Biol. 2013;33:413–9.
• Ras RT, van der Schouw YT, Trautwein EA, Sioen I, Dalmeijer GW, Zock PL, et al. Intake of phytosterols from natural sources and risk of cardiovascular disease in the European Prospective Investigation into Cancer and Nutrition-the Netherlands (EPIC-NL) population. Eur J Prev Cardiol. 2015;22:1067–75. In this observational prospective study enrolling 35,597 Dutch men and women, the oral intake of plant sterol was not associated with a significant reduction of CV disease risk.
Klingberg S, Ellegård L, Johansson I, Jansson JH, Hallmans G, Winkvist A. Dietary intake of naturally occurring plant sterols is related to a lower risk of a first myocardial infarction in men but not in women in northern Sweden. J Nutr. 2013;143:1630–5.
Gylling H, Plat J, Turley S, Ginsberg HN, Ellegård L, Jessup W, et al. Plant sterols and plant stanols in the management of dyslipidaemia and prevention of cardiovascular disease. Atherosclerosis. 2014;232:346–60.
Tsao R. Chemistry and biochemistry of dietary polyphenols. Nutrients. 2010;2:1231–46.
Baba S, Natsume M, Yasuda A, Nakamura Y, Tamura T, Osakabe N, et al. Plasma LDL and HDL cholesterol and oxidized LDL concentrations are altered in normo- and hypercholesterolemic humans after intake of different levels of cocoa powder. J Nutr. 2007;137:1436–41.
Xia EQ, Deng GF, Guo YJ, Li HB. Biological activities of polyphenols from grapes. Int J Mol Sci. 2010;11:622–46.
McDougall GJ, Stewart D. The inhibitory effects of berry polyphenols on digestive enzymes. Biofactors. 2005;23:189–95.
Shishikura Y, Khokhar S, Murray BS. Effects of tea polyphenols on emulsification of olive oil in a small intestine model system. J Agric Food Chem. 2006;54:1906–13.
Babu PV, Liu D. Green tea catechins and cardiovascular health: an update. Curr Med Chem. 2008;15:1840–50.
Onakpoya I, Spencer E, Heneghan C, Thompson M. The effect of green tea on blood pressure and lipid profile: a systematic review and meta-analysis of randomized clinical trials. Nutr Metab Cardiovasc Dis. 2014;24:823–36.
Park CS, Kim W, Woo JS, Ha SJ, Kang WY, Hwang SH, et al. Green tea consumption improves endothelial function but not circulating endothelial progenitor cells in patients with chronic renal failure. Int J Cardiol. 2010;145(2):261.
• Lin QF, Qiu CS, Wang SL, Huang LF, Chen ZY, Chen Y, et al. Cross-sectional study of the relationship between habitual tea consumption and arterial stiffness. J Am Coll Nutr. 2016;35:354–61. In this observational study, habitual tea consumption (> 10 g/day for more than 6 years) was associated with a significant improvement of arterial stiffness.
• Ding S, Jiang J, Yu P, Zhang G, Zhang G, Liu X. Green tea polyphenol treatment attenuates atherosclerosis in high-fat diet-fed apolipoprotein E-knockout mice via alleviating dyslipidemia and up-regulating autophagy. PLoS One. 2017;12:e0181666. In apolipoprotein E-deficient mice, green tea polyphenol supplementation reduced blood levels of oxidized LDL cholesterol and expression of autophagy markers in arterial wall.
•• Zhang C, Qin YY, Wei X, Yu FF, Zhou YH, He J. Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta-analysis of prospective observational studies. Eur J Epidemiol. 2015;30:103–13. In this meta-analysis of 22 prospective studies, an increase in tea consumption by 3 cups per day was associated with a significant reduction of CV risk.
Peters U, Poole C, Arab L. Does tea affect cardiovascular disease? A meta-analysis. Am J Epidemiol. 2001;154:495–503.
Grassi D, Necozione S, Lippi C, Croce G, Valeri L, Pasqualetti P, et al. Cocoa reduces blood pressure and insulin resistance and improves endothelium-dependent vasodilation in hypertensives. Hypertension. 2005;46:398–405.
• Grassi D, Desideri G, Necozione S, di Giosia P, Barnabei R, Allegaert L, et al. Cocoa consumption dose-dependently improves flow-mediated dilation and arterial stiffness decreasing blood pressure in healthy individuals. Hypertens. 2015;33:294–303. In this randomized, double-blind, cross-over study, the daily intake of 10 mg of cocoa was associated with a dose-dependent reduction of FMD.
Recio-Rodríguez JI, Gómez-Marcos MA, Patino-Alonso MC, Agudo-Conde C, Rodríguez-Sánchez E, García-Ortiz L, et al. Cocoa intake and arterial stiffness in subjects with cardiovascular risk factors. Nutr J. 2012;11:8.
Kurosawa T, Itoh F, Nozaki A, Nakano Y, Katsuda S, Osakabe N, et al. Suppressive effect of cocoa powder on atherosclerosis in Kurosawa and Kusanagi-hypercholesterolemic rabbits. J Atheroscler Thromb. 2005;12:20–8.
Arranz S, Valderas-Martinez P, Chiva-Blanch G, Casas R, Urpi-Sarda M, Lamuela-Raventos RM, et al. Cardioprotective effects of cocoa: clinical evidence from randomized clinical intervention trials in humans. Mol Nutr Food Res. 2013;57:936–47.
Buijsse B, Feskens EJ, Kok FJ, Kromhout D. Cocoa intake, blood pressure, and cardiovascular mortality: the Zutphen Elderly Study. Arch Intern Med. 2006;166:411–7.
Sahebkar A. Effects of resveratrol supplementation on plasma lipids: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2013;71:822–35.
Bonnefont-Rousselot D. Resveratrol and cardiovascular diseases. Nutrients. 2016;8:250.
Bonechi C, Lamponi S, Donati A, Tamasi G, Consumi M, Leone G, et al. Effect of resveratrol on platelet aggregation by fibrinogen protection. Biophys Chem. 2017;222:41–8.
Wong RH, Berry NM, Coates AM, Buckley JD, Bryan J, Kunz I, et al. Chronic resveratrol consumption improves brachial flow-mediated dilatation in healthy obese adults. J Hypertens. 2013;31:1819–27.
• van der Made SM, Plat J, Mensink RP. Trans-resveratrol supplementation and endothelial function during the fasting and postprandial phase: a randomized placebo-controlled trial in overweight and slightly obese participants. Nutrients. 2017;9:596. In this interventional study, the oral intake of resveratrol 75 mg/bid did not improve endothelial function.
• Imamura H, Yamaguchi T, Nagayama D, Saiki A, Shirai K, Tatsuno I. Resveratrol ameliorates arterial stiffness assessed by cardio-ankle vascular index in patients with type 2 diabetes mellitus. Int Heart J. 2017;58:577–83. In this study, a 12-week oral supplementation with resveratrol 100 mg improved arterial stiffness in patients with type 2 diabetes mellitus.
•• Sahebkar A, Serban C, Ursoniu S, Wong ND, Muntner P, Graham IM, et al. Lack of efficacy of resveratrol on C-reactive protein and selected cardiovascular risk factors—results from a systematic review and meta-analysis of randomized controlled trials. Int J Cardiol. 2015;189:47–55. This meta-analysis of 10 randomized clinical trials did not show any significant impact of resveratrol supplementation on plasma lipids, markers of systemic inflammation, and blood pressure.
•• Fogacci F, Tocci G, Presta V, Fratter A, Borghi C, Cicero AFG. Effect of resveratrol on blood pressure: a systematic review and meta-analysis of randomized, controlled, clinical trials. Crit Rev Food Sci Nutr. 2018;23:1–14. This meta-analysis of randomized clinical trials revealed a significant impact of oral supplementation with resveratrol at high daily dosage (≥ 300 mg/day) on blood pressure levels.
Wang Z, Zou J, Cao K, Hsieh TC, Huang Y, Wu JM. Dealcoholized red wine containing known amounts of resveratrol suppresses atherosclerosis in hypercholesterolemic rabbits without affecting plasma lipid levels. Int J Mol Med. 2005;16:533–40.
Wilson T, Knight TJ, Beitz DC, Lewis DS, Engen RL. Resveratrol promotes atherosclerosis in hypercholesterolemic rabbits. Life Sci. 1996;59:PL15–21.
Vidavalur R, Otani H, Singal PK, Maulik N. Significance of wine and resveratrol in cardiovascular disease: French paradox revisited. Exp Clin Cardiol. 2006;11:217–25.
Qin Y, Xia M, Ma J, Hao Y, Liu J, Mou H, et al. Anthocyanin supplementation improves serum LDL- and HDL-cholesterol concentrations associated with the inhibition of cholesteryl ester transfer protein in dyslipidemic subjects. Am J Clin Nutr. 2009;90:485–92.
Jennings A, Welch AA, Fairweather-Tait SJ, Kay C, Minihane AM, Chowienczyk P, et al. Higher anthocyanin intake is associated with lower arterial stiffness and central blood pressure in women. Am J Clin Nutr. 2012;96:781–8.
Zhu Y, Xia M, Yang Y, Liu F, Li Z, Hao Y, et al. Purified anthocyanin supplementation improves endothelial function via NO-cGMP activation in hypercholesterolemic individuals. Clin Chem. 2011;57:1524–33.
Mauray A, Felgines C, Morand C, Mazur A, Scalbert A, Milenkovic D. Bilberry anthocyanin-rich extract alters expression of genes related to atherosclerosis development in aorta of apo E-deficient mice. Nutr Metab Cardiovasc Dis. 2012;22:72–80.
•• Luís Â, Domingues F, Pereira L. Association between berries intake and cardiovascular diseases risk factors: a systematic review with meta-analysis and trial sequential analysis of randomized controlled trials. Food Funct. 2018;9:740–757. In this meta-analysis of randomized controlled trials, oral intake of berries reduced significantly plasma levels of LDL cholesterol.
Hori G, Wang MF, Chan YC, Komatsu T, Wong Y, Chen TH, et al. Soy protein hydrolyzate with bound phospholipids reduces serum cholesterol levels in hypercholesterolemic adult male volunteers. Biosci Biotechnol Biochem. 2001;65:72–8.
Taku K, Umegaki K, Sato Y, Taki Y, Endoh K, Watanabe S. Soy isoflavones lower serum total and LDL cholesterol in humans: a meta-analysis of 11 randomized controlled trials. Am J Clin Nutr. 2007;85:1148–56.
Padhi EM, Blewett HJ, Duncan AM, Guzman RP, Hawke A, Seetharaman K, et al. Whole soy flour incorporated into a muffin and consumed at 2 doses of soy protein does not lower LDL cholesterol in a randomized, double-blind controlled trial of hypercholesterolemic adults. J Nutr. 2015;145:2665–74.
Anderson JW, Johnstone BM, Cook-Newell ME. Meta-analysis of the effects of soy protein intake on serum lipids. N Engl J Med. 1995;333:276–82.
Harland JI, Haffner TA. Systematic review, meta-analysis and regression of randomised controlled trials reporting an association between an intake of circa 25 g soy a protein per day and blood cholesterol. Atherosclerosis. 2008;200:13–27.
•• Tokede OA, Onabanjo TA, Yansane A, Gaziano JM, Djoussé L. Soya products and serum lipids: a meta-analysis of randomised controlled trials. Br J Nutr. 2015;114:831–43. In this meta-analysis of randomized controlled trials, oral consumption of soy product was associated with a significant reduction in plasma LDL cholesterol levels.
Ramdath DD, Padhi EM, Sarfaraz S, Renwick S, Duncan AM. Beyond the cholesterol-lowering effect of soy protein: a review of the effects of dietary soy and its constituents on risk factors for cardiovascular disease. Nutrients. 2017;9
Sakamoto Y, Kanatsu J, Toh M, Naka A, Kondo K, Iida K. The dietary isoflavone daidzein reduces expression of pro-inflammatory genes through PPARα/γ and JNK pathways in adipocyte and macrophage co-cultures. PLoS One. 2016;11:e0149676.
Lesinski GB, Reville PK, Mace TA, Young GS, Ahn-Jarvis J, Thomas-Ahner J, et al. Consumption of soy isoflavone enriched bread in men with prostate cancer is associated with reduced proinflammatory cytokines and immunosuppressive cells. Cancer Prev Res (Phila). 2015;8:1036–44.
Garrido A, De la Maza MP, Hirsch S, Valladares L. Soy isoflavones affect platelet thromboxane A2 receptor density but not plasma lipids in menopausal women. Maturitas. 2006;54:270–6.
Adams MR, Golden DL, Anthony MS, Register TC, Williams JK. The inhibitory effect of soy protein isolate on atherosclerosis in mice does not require the presence of LDL receptors or alteration of plasma lipoproteins. J Nutr. 2002;132:43–9.
Beavers DP, Beavers KM, Miller M, Stamey J, Messina MJ. Exposure to isoflavone-containing soy products and endothelial function: a Bayesian meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. 2012;22:182–91.
Törmälä R, Appt S, Clarkson TB, Groop PH, Rönnback M, Ylikorkala O, et al. Equol production capability is associated with favorable vascular function in postmenopausal women using tibolone; no effect with soy supplementation. Atherosclerosis. 2008;198:174–8.
Clerici C, Setchell KD, Battezzati PM, Pirro M, Giuliano V, Asciutti S, et al. Pasta naturally enriched with isoflavone aglycons from soy germ reduces serum lipids and improves markers of cardiovascular risk. J Nutr. 2007;137:2270–8.
Liu ZM, Ho SC, Chen YM, Tomlinson B, Ho S, To K, et al. Effect of whole soy and purified daidzein on ambulatory blood pressure and endothelial function—a 6-month double-blind, randomized controlled trial among Chinese postmenopausal women with prehypertension. Eur J Clin Nutr. 2015;69:1161–8.
Richter CK, Skulas-Ray AC, Fleming JA, Link CJ, Mukherjea R, Krul ES, et al. Effects of isoflavone-containing soya protein on ex vivo cholesterol efflux, vascular function and blood markers of CVD risk in adults with moderately elevated blood pressure: a dose-response randomised controlled trial. Br J Nutr. 2017;117:1403–13.
Cuevas AM, Irribarra VL, Castillo OA, Yañez MD, Germain AM. Isolated soy protein improves endothelial function in postmenopausal hypercholesterolemic women. Eur J Clin Nutr. 2003;57:889–94.
Reverri EJ, LaSalle CD, Franke AA, Steinberg FM. Soy provides modest benefits on endothelial function without affecting inflammatory biomarkers in adults at cardiometabolic risk. Mol Nutr Food Res. 2015;59:323–33.
Clerici C, Nardi E, Battezzati PM, Asciutti S, Castellani D, Corazzi N, et al. Novel soy germ pasta improves endothelial function, blood pressure, and oxidative stress in patients with type 2 diabetes. Diabetes Care. 2011;34:1946–8.
Teede HJ, McGrath BP, DeSilva L, Cehun M, Fassoulakis A, Nestel PJ. Isoflavones reduce arterial stiffness: a placebo-controlled study in men and postmenopausal women. Arterioscler Thromb Vasc Biol. 2003;23:1066–71.
van Nielen M, Feskens EJ, Rietman A, Siebelink E, Mensink M. Partly replacing meat protein with soy protein alters insulin resistance and blood lipids in postmenopausal women with abdominal obesity. J Nutr. 2014;144(9):1423.
Nestel PJ, Yamashita T, Sasahara T, Pomeroy S, Dart A, Komesaroff P, et al. Soy isoflavones improve systemic arterial compliance but not plasma lipids in menopausal and perimenopausal women. Arterioscler Thromb Vasc Biol. 1997;17:3392–8.
Teede H, Dalais F, Kotsopoulos D, Liang YL, Davis S, Mc Grath B. Dietary soy has both beneficial and potentially adverse cardiovascular effects: a placebo-controlled study in men and postmenopausal women. J Clin Endocrinol Metab. 2001;86:3053–60.
Meléndez GC, Register TC, Appt SE, Clarkson TB, Franke AA, Kaplan JR. Beneficial effects of soy supplementation on postmenopausal atherosclerosis are dependent on pretreatment stage of plaque progression. Menopause. 2015;22:289–96.
Hodis HN, Mack WJ, Kono N, Azen SP, Shoupe D, Hwang-Levine J, et al. Isoflavone soy protein supplementation and atherosclerosis progression in healthy postmenopausal women: a randomized controlled trial. Stroke. 2011;42:3168–75.
Liu J, Sun LL, He LP, Ling WH, Liu ZM, Chen YM. Soy food consumption, cardiometabolic alterations and carotid intima-media thickness in Chinese adults. Nutr Metab Cardiovasc Dis. 2014;24:1097–104.
Zhang B, Chen YM, Huang LL, Zhou XX, Chen CG, Ye YB, et al. Greater habitual soyfood consumption is associated with decreased carotid intima-media thickness and better plasma lipids in Chinese middle-aged adults. Atherosclerosis. 2008;198:403–11.
Shimazu T, Kuriyama S, Hozawa A, Ohmori K, Sato Y, Nakaya N, et al. Dietary patterns and cardiovascular disease mortality in Japan: a prospective cohort study. Int J Epidemiol. 2007;36:600–9.
Liu ZM, Ho SC, Chen YM, Ho S, To K, Tomlinson B, et al. Whole soy, but not purified daidzein, had a favorable effect on improvement of cardiovascular risks: a 6-month randomized, double-blind, and placebo-controlled trial in equol-producing postmenopausal women. Mol Nutr Food Res. 2014;58:709–17.
Nagata C, Wada K, Tamura T, Konishi K, Goto Y, Koda S, et al. Dietary soy and natto intake and cardiovascular disease mortality in Japanese adults: the Takayama study. Am J Clin Nutr. 2017;105:426–31.
•• Yan Z, Zhang X, Li C, Jiao S, Dong W. Association between consumption of soy and risk of cardiovascular disease: a meta-analysis of observational studies. Eur J Prev Cardiol. 2017;24:735–47. In this meta-analysis of observational studies, a significant negative association between soy consumption and cardiovascular risk was found.
•• Lou D, Li Y, Yan G, Bu J, Wang H. Soy consumption with risk of coronary heart disease and stroke: a meta-analysis of observational studies. Neuroepidemiology. 2016;46:242–52. In this meta-analysis of observational studies, no significant association between soy isoflavone intake and the risk of stroke and coronary heart disease was found.
Liu J, Zhang J, Shi Y, Grimsgaard S, Alraek T, Fønnebø V. Chinese red yeast rice (Monascus purpureus) for primary hyperlipidemia: a meta-analysis of randomized controlled trials. Chin Med. 2006;1:4.
Li Y, Jiang L, Jia Z, Xin W, Yang S, Yang Q, et al. A meta-analysis of red yeast rice: an effective and relatively safe alternative approach for dyslipidemia. PLoS One. 2014;9:e98611.
Gerards MC, Terlou RJ, Yu H, Koks CH, Gerdes VE. Traditional Chinese lipid-lowering agent red yeast rice results in significant LDL reduction but safety is uncertain—a systematic review and meta-analysis. Atherosclerosis. 2015;240:415–23.
Xiong X, Wang P, Li X, Zhang Y, Li S. The effects of red yeast rice dietary supplement on blood pressure, lipid profile, and C-reactive protein in hypertension: a systematic review. Crit Rev Food Sci Nutr. 2017;57:1831–51.
Xu B, Cheng W, Lu X. The effect of Xuezhikang on oxidation of low-density lipoproteins in vitro. Zhonghua Nei Ke Za Zhi. 1999;38:520–2.
Liu L, Zhao SP, Cheng YC, Li YL. Xuezhikang decreases serum lipoprotein(a) and C-reactive protein concentrations in patients with coronary heart disease. Clin Chem. 2003;49:1347–52.
Lin CP, Chen YH, Chen JW, Leu HB, Liu TZ, Liu PL, et al. Cholestin (Monascus purpureus rice) inhibits homocysteine-induced reactive oxygen species generation, nuclear factor-kappaB activation, and vascular cell adhesion molecule-1 expression in human aortic endothelial cells. J Biomed Sci. 2008;15:183–96.
Hsieh YL, Yeh YH, Lee YT, Huang CY. Protective effects of cholestin on ethanol induced oxidative stress in rats. J Sci Food Agric. 2015;95:799–808.
Lin CP, Lin YL, Huang PH, Tsai HS, Chen YH. Inhibition of endothelial adhesion molecule expression by Monascus purpureus-fermented rice metabolites, monacolin K, ankaflavin, and monascin. J Sci Food Agric. 2011;91:1751–8.
Zhu XY, Li P, Yang YB, Liu ML. Xuezhikang, extract of red yeast rice, improved abnormal hemorheology, suppressed caveolin-1 and increased eNOS expression in atherosclerotic rats. PLoS One. 2013;8:e62731.
Li P, Yang Y, Liu M. Xuezhikang, extract of red yeast rice, inhibited tissue factor and hypercoagulable state through suppressing nicotinamide adenine dinucleotide phosphate oxidase and extracellular signal-regulated kinase activation. J Cardiovasc Pharmacol. 2011;58:307–18.
Cicero AF, Derosa G, Parini A, Maffioli P, D'Addato S, Reggi A, et al. Red yeast rice improves lipid pattern, high-sensitivity C-reactive protein, and vascular remodeling parameters in moderately hypercholesterolemic Italian subjects. Nutr Res. 2013;33(8):622.
Zhao SP, Liu L, Cheng YC, Shishehbor MH, Liu MH, Peng DQ, et al. Xuezhikang, an extract of cholestin, protects endothelial function through antiinflammatory and lipid-lowering mechanisms in patients with coronary heart disease. Circulation. 2004;110:915–20.
• Zheng J, Xiao T, Ye P, Miao D, WH. Xuezhikang reduced arterial stiffness in patients with essential hypertension: a preliminary study. Braz J Med Biol Res. 2017:50–e6363. In this randomized controlled trial, oral supplementation with xuezhikang 1200 mg/day improved arterial stiffness in hypertensive patients.
• Shen L, Sun Z, Chu S, Cai Z, Nie P, Wu C, et al. Xuezhikang, an extract from red yeast rice, attenuates vulnerable plaque progression by suppressing endoplasmic reticulum stress-mediated apoptosis and inflammation. PLoS One. 2017;12:e0188841. In apolipoprotein E-deficient mice, xuezhikang administration reduced carotid vulnerable plaque progression and rupture.
• Wu M, Zhang WG, Liu LT. Red yeast rice prevents atherosclerosis through regulating inflammatory signaling pathways. Chin J Integr Med. 2017;23:689–95. In apolipoprotein E-deficient mice, red yeast rice treatment reduced plasma levels of different markers of systemic inflammation and decreased the expression of matrix metalloproteinase-9 in aortic wall.
Xie X, Wang Y, Zhang S, Zhang G, Xu Y, Bi H, et al. Chinese red yeast rice attenuates the development of angiotensin II-induced abdominal aortic aneurysm and atherosclerosis. J Nutr Biochem. 2012;23:549–56.
Lu Z, Kou W, Du B, Wu Y, Zhao S, Brusco OA, et al. Effect of Xuezhikang, an extract from red yeast Chinese rice, on coronary events in a Chinese population with previous myocardial infarction. Am J Cardiol. 2008;101:1689–93.
Kong W, Wei J, Abidi P, Lin M, Inaba S, Li C, et al. Berberine is a novel cholesterol-lowering drug working through a unique mechanism distinct from statins. Nat Med. 2004;10:1344–51.
Dong H, Zhao Y, Zhao L, Lu F. The effects of berberine on blood lipids: a systemic review and meta-analysis of randomized controlled trials. Planta Med. 2013;79:437–46.
Lan J, Zhao Y, Dong F, Yan Z, Zheng W, Fan J, et al. Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension. J Ethnopharmacol. 2015;161:69–81.
Dong H, Wang N, Zhao L, Lu F. Berberine in the treatment of type 2 diabetes mellitus: a systemic review and meta-analysis. Evid Based Complement Alternat Med. 2012;2012:591654.
Qiang X, Xu L, Zhang M, Zhang P, Wang Y, Wang Y, et al. Demethyleneberberine attenuates non-alcoholic fatty liver disease with activation of AMPK and inhibition of oxidative stress. Biochem Biophys Res Commun. 2016;472:603–9.
Li Z, Geng YN, Jiang JD, Kong WJ. Antioxidant and anti-inflammatory activities of berberine in the treatment of diabetes mellitus. Evid Based Complement Alternat Med. 2014;2014:289264.
Meng S, Wang LS, Huang ZQ, Zhou Q, Sun YG, Cao JT, et al. Berberine ameliorates inflammation in patients with acute coronary syndrome following percutaneous coronary intervention. Clin Exp Pharmacol Physiol. 2012;39:406–11.
Pirillo A, Catapano AL. Berberine, a plant alkaloid with lipid- and glucose-lowering properties: from in vitro evidence to clinical studies. Atherosclerosis. 2015;243:449–61.
Ma YG, Liang L, Zhang YB, Wang BF, Bai YG, Dai ZJ, et al. Berberine reduced blood pressure and improved vasodilation in diabetic rats. J Mol Endocrinol. 2017;59:191–204.
Wang J, Guo T, Peng QS, Yue SW, Wang SX. Berberine via suppression of transient receptor potential vanilloid 4 channel improves vascular stiffness in mice. J Cell Mol Med. 2015;19:2607–16.
Caliceti C, Rizzo P, Ferrari R, Fortini F, Aquila G, Leoncini E, et al. Novel role of the nutraceutical bioactive compound berberine in lectin-like OxLDL receptor 1-mediated endothelial dysfunction in comparison to lovastatin. Nutr Metab Cardiovasc Dis. 2017;27:552–63.
Xu MG, Wang JM, Chen L, Wang Y, Yang Z, Tao J. Berberine-induced mobilization of circulating endothelial progenitor cells improves human small artery elasticity. J Hum Hypertens. 2008;22:389–93.
Cheng F, Wang Y, Li J, Su C, Wu F, Xia WH, et al. Berberine improves endothelial function by reducing endothelial microparticles-mediated oxidative stress in humans. Int J Cardiol. 2013;167:936–42.
Li K, Yao W, Zheng X, Liao K. Berberine promotes the development of atherosclerosis and foam cell formation by inducing scavenger receptor A expression in macrophage. Cell Res. 2009;19:1006–17.
Wan Q, Liu Z, Yang Y, Cui X. Suppressive effects of berberine on atherosclerosis via downregulating visfatin expression and attenuating visfatin-induced endothelial dysfunction. Int J Mol Med. 2018;
• Feng M, Zou Z, Zhou X, Hu Y, Ma H, Xiao Y, et al. Comparative effect of berberine and its derivative 8-cetylberberine on attenuating atherosclerosis in ApoE-/- mice. Int Immunopharmacol. 2017;43:195–202. In apolipoprotein E-deficient mice, a 12-week oral supplementation with either berberine or 8-cetylberberine reduced the atherosclerotic plaque area of the aorta.
Li Y, Wang P, Chai MJ, Yang F, Li HS, Zhao J, et al. Effects of berberine on serum inflammatory factors and carotid atherosclerotic plaques in patients with acute cerebral ischemic stroke. Zhongguo Zhong Yao Za Zhi. 2016;41:4066–71.
Yang YS, Su YF, Yang HW, Lee YH, Chou JI, Ueng KC. Lipid-lowering effects of curcumin in patients with metabolic syndrome: a randomized, double-blind, placebo-controlled trial. Phytother Res. 2014;28:1770–7.
Panahi Y, Khalili N, Hosseini MS, Abbasinazari M, Sahebkar A. Lipid-modifying effects of adjunctive therapy with curcuminoids-piperine combination in patients with metabolic syndrome: results of a randomized controlled trial. Complement Ther Med. 2014;22:851–7.
Sahebkar A. A systematic review and meta-analysis of randomized controlled trials investigating the effects of curcumin on blood lipid levels. Clin Nutr. 2014;33:406–14.
•• Simental-Mendía LE, Pirro M, Gotto AM Jr, Banach M, Atkin SL, Majeed M, Sahebkar A. Lipid-modifying activity of curcuminoids: a systematic review and meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2017;29(Nov):1–10. This meta-analysis of 20 randomized clinical trials enrolling 1427 patients showed that curcuminoid treatment did not reduce significantly plasma LDL cholesterol levels.
Menon VP, Sudheer AR. Antioxidant and anti-inflammatory properties of curcumin. Adv Exp Med Biol. 2007;595:105–25.
Ghandadi M, Sahebkar A. Curcumin: an effective inhibitor of interleukin-6. Curr Pharm Des. 2017;23:921–31.
•• Sahebkar A, Cicero AFG, Simental-Mendía LE, Aggarwal BB, Gupta SC. Curcumin downregulates human tumor necrosis factor-α levels: a systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2016;107:234–42. This meta-analysis of eight randomized clinical trials reported a significant curcumin-mediated reduction of circulating TNF-α concentration.
Sangartit W, Kukongviriyapan U, Donpunha W, Pakdeechote P, Kukongviriyapan V, Surawattanawan P, et al. Tetrahydrocurcumin protects against cadmium-induced hypertension, raised arterial stiffness and vascular remodeling in mice. PLoS One. 2014;9:e114908.
Karimian MS, Pirro M, Johnston TP, Majeed M, Sahebkar A. Curcumin and endothelial function: evidence and mechanisms of protective effects. Curr Pharm Des. 2017;23:2462–73.
Campbell MS, Fleenor BS. The emerging role of curcumin for improving vascular dysfunction: a review. Crit Rev Food Sci Nutr 2017;29(Jun):1–10.
• Santos-Parker JR, Strahler TR, Bassett CJ, Bispham NZ, Chonchol MB, Seals DR. Curcumin supplementation improves vascular endothelial function in healthy middle-aged and older adults by increasing nitric oxide bioavailability and reducing oxidative stress. Aging (Albany NY). 2017;9:187–208. In this interventional study, a 12-week oral supplementation with curcumin improved resistance artery endothelial function by increasing nitric oxide bioavailability and reducing oxidative stress.
• Oliver JM, Stoner L, Rowlands DS, Caldwell AR, Sanders E, Kreutzer A, et al. Novel form of curcumin improves endothelial function in young, healthy individuals: a double-blind placebo controlled study. J Nutr Metab. 2016;2016:1089653. In this interventional study, oral supplementation with curcumin was associated with a dose-dependent improvement of endothelial function.
Shin SK, Ha TY, McGregor RA, Choi MS. Long-term curcumin administration protects against atherosclerosis via hepatic regulation of lipoprotein cholesterol metabolism. Mol Nutr Food Res. 2011;55:1829–40.
• Zhang S, Zou J, Li P, Zheng X, Feng D. Curcumin protects against atherosclerosis in apolipoprotein e-knockout mice by inhibiting toll-like receptor 4 expression. J Agric Food Chem. 2018;66:449–56. In apolipoprotein E-deficient mice, curcumin reduced atherosclerosis progression through immunomodulatory effects.
Momtazi AA, Shahabipour F, Khatibi S, Johnston TP, Pirro M, Sahebkar A. Curcumin as a microRNA regulator in cancer: a review. Rev Physiol Biochem Pharmacol. 2016;171:1–38.
Bianconi V, Sahebkar A, Atkin SL, Pirro M. The regulation and importance of monocyte chemoattractant protein-1. Curr Opin Hematol. 2018;25:44–51.
Ganjali S, Blesso CN, Banach M, Pirro M, Majeed M, Sahebkar A. Effects of curcumin on HDL functionality. Pharmacol Res. 2017;119:208–18.
Chung LY. The antioxidant properties of garlic compounds: allyl cysteine, alliin, allicin, and allyl disulfide. J Med Food. 2006;9:205–13.
Mikaili P, Maadirad S, Moloudizargari M, Aghajanshakeri S, Sarahroodi S. Therapeutic uses and pharmacological properties of garlic, shallot, and their biologically active compounds. Iran J Basic Med Sci. 2013;16:1031–48.
Lau KK, Chan YH, Wong YK, Teo KC, Yiu KH, Liu S, et al. Garlic intake is an independent predictor of endothelial function in patients with ischemic stroke. J Nutr Health Aging. 2013;17:600–4.
• Mahdavi-Roshan M, Mirmiran P, Arjmand M, Nasrollahzadeh J. Effects of garlic on brachial endothelial function and capacity of plasma to mediate cholesterol efflux in patients with coronary artery disease. Anatol J Cardiol. 2017;18:116–21. In this randomized, placebo-controlled trial, oral supplementation with aged garlic extract improved endothelial function and reduced hs-CRP levels.
• Atkin M, Laight D, Cummings MH. The effects of garlic extract upon endothelial function, vascular inflammation, oxidative stress and insulin resistance in adults with type 2 diabetes at high cardiovascular risk. A pilot double blind randomized placebo controlled trial. J Diabet Complications. 2016;30:723–7. In this double-blind, placebo controlled, crossover study, oral supplementation with aged garlic extract did not significantly improve endothelial function.
Turner B, Mølgaard C, Marckmann P. Effect of garlic (Allium sativum) powder tablets on serum lipids, blood pressure and arterial stiffness in normo-lipidaemic volunteers: a randomised, double-blind, placebo-controlled trial. Br J Nutr. 2004;92:701–6.
• Ried K, Travica N, Sali A. The effect of aged garlic extract on blood pressure and other cardiovascular risk factors in uncontrolled hypertensives: the AGE at Heart trial. Integr Blood Press Control. 2016;9:9–21. In this double-blind, randomized, placebo-controlled trial, oral supplementation with aged garlic extract improved arterial stiffness and markers of systemic inflammation.
Xiong XJ, Wang PQ, Li SJ, Li XK, Zhang YQ, Wang J. Garlic for hypertension: a systematic review and meta-analysis of randomized controlled trials. Phytomedicine. 2015;22:352–61.
Budoff M. Aged garlic extract retards progression of coronary artery calcification. J Nutr. 2006;136:741S–4S.
• Matsumoto S, Nakanishi R, Li D, Alani A, Rezaeian P, Prabhu S, et al. Aged garlic extract reduces low attenuation plaque in coronary arteries of patients with metabolic syndrome in a prospective randomized double-blind study. J Nutr. 2016;146:427S–32S. In this interventional study, oral supplementation with aged garlic extract reduced low-attenuation plaque in coronary arteries of patients with metabolic syndrome.
Karagodin VP, Sobenin IA, Orekhov AN. Antiatherosclerotic and cardioprotective effects of time-released garlic powder pills. Curr Pharm Des. 2016;22:196–213.
•• Sahebkar A, Pirro M, Banach M, Mikhailidis DP, Atkin SL, Cicero AFG. Lipid-lowering activity of artichoke extracts: a systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2017;13:1–8. In this meta-analysis of nine randomized clinical trials, enrolling 702 subjects, oral supplementation with artichoke extract was associated with a significant reduction of plasma LDL cholesterol and triglyceride levels.
Pérez-García F, Adzet T, Cañigueral S. Activity of artichoke leaf extract on reactive oxygen species in human leukocytes. Free Radic Res. 2000;33(5):661.
Lupattelli G, Marchesi S, Lombardini R, Roscini AR, Trinca F, Gemelli F, et al. Artichoke juice improves endothelial function in hyperlipemia. Life Sci. 2004;76:775–82.
Rossoni G, Grande S, Galli C, Visioli F. Wild artichoke prevents the age-associated loss of vasomotor function. J Agric Food Chem. 2005;53:10291–6.
•• Toth PP, Patti AM, Nikolic D, Giglio RV, Castellino G, Biancucci T, et al. Bergamot reduces plasma lipids, atherogenic small dense LDL, and subclinical atherosclerosis in subjects with moderate hypercholesterolemia: a 6 months prospective study. Front Pharmacol. 2015;6:29. This is the first interventional study investigating the effects of oral supplementation with bergamot flavonoids on lipids and subclinical atherosclerosis.
Risitano R, Currò M, Cirmi S, Ferlazzo N, Campiglia P, Caccamo D, et al. Flavonoid fraction of bergamot juice reduces LPS-induced inflammatory response through SIRT1-mediated NF-κB inhibition in THP-1 monocytes. PLoS One. 2014;9:e107431.
•• Jolfaie NR, Rouhani MH, Surkan PJ, Siassi F, Azadbakht L. Rice bran oil decreases total and LDL cholesterol in humans: a systematic review and meta-analysis of randomized controlled clinical trials. Horm Metab Res. 2016;48:417–26. In this meta-analysis of 11 randomized clinical trials, rice bran oil consumption resulted in a significant reduction of LDL cholesterol levels.
Cicero AF, Gaddi A. Rice bran oil and gamma-oryzanol in the treatment of hyperlipoproteinaemias and other conditions. Phytother Res. 2001;15:277–89.
Sakai S, Murata T, Tsubosaka Y, Ushio H, Hori M, Ozaki H. γ-Oryzanol reduces adhesion molecule expression in vascular endothelial cells via suppression of nuclear factor-κB activation. J Agric Food Chem. 2012;60:3367–72.
Rong N, Ausman LM, Nicolosi RJ. Oryzanol decreases cholesterol absorption and aortic fatty streaks in hamsters. Lipids. 1997;32:303–9.
Hiramatsu K, Tani T, Kimura Y, Izumi S, Nakane PK. Effect of gamma-oryzanol on atheroma formation in hypercholesterolemic rabbits. Tokai J Exp Clin Med. 1990;15:299–305.
Cheong SH, Kim MY, Sok DE, Hwang SY, Kim JH, Kim HR, et al. Spirulina prevents atherosclerosis by reducing hypercholesterolemia in rabbits fed a high-cholesterol diet. J Nutr Sci Vitaminol (Tokyo). 2010;56:34–40.
• Szulinska M, Gibas-Dorna M, Miller-Kasprzak E, Suliburska J, Miczke A, Walczak-Gałezewska M, et al. Spirulina maxima improves insulin sensitivity, lipid profile, and total antioxidant status in obese patients with well-treated hypertension: a randomized double-blind placebo-controlled study. Eur Rev Med Pharmacol Sci. 2017;21:2473–81. In this randomized clinical trial, oral supplementation with spirulina 2 g reduced significantly body mass index, plasma LDL cholesterol levels, and interleukin-6 concentrations and improved significantly insulin sensitivity.
• Miczke A, Szulińska M, Hansdorfer-Korzon R, Kręgielska-Narożna M, Suliburska J, Walkowiak J, et al. Effects of spirulina consumption on body weight, blood pressure, and endothelial function in overweight hypertensive Caucasians: a double-blind, placebo-controlled, randomized trial. Eur Rev Med Pharmacol Sci. 2016;20:150–6. In this randomized clinical trial, spirulina 2 g/day improved body mass index, blood pressure, and endothelial function in overweight hypertensive patients.
•• Derakhshande-Rishehri SM, Mansourian M, Kelishadi R, Heidari-Beni M. Association of foods enriched in conjugated linoleic acid (CLA) and CLA supplements with lipid profile in human studies: a systematic review and meta-analysis. Public Health Nutr. 2015;18:2041–54. This meta-analysis showed that oral supplementation with conjugated linoleic acid reduced significantly LDL cholesterol levels.
Taylor JS, Williams SR, Rhys R, James P, Frenneaux MP. Conjugated linoleic acid impairs endothelial function. Arterioscler Thromb Vasc Biol. 2006;26:307–12.
Sluijs I, Plantinga Y, de Roos B, Mennen LI, Bots ML. Dietary supplementation with cis-9,trans-11 conjugated linoleic acid and aortic stiffness in overweight and obese adults. Am J Clin Nutr. 2010;91:175–83.
Lee KN, Kritchevsky D, Pariza MW. Conjugated linoleic acid and atherosclerosis in rabbits. Atherosclerosis. 1994;108:19–25.
Raff M, Tholstrup T, Sejrsen K, Straarup EM, Wiinberg N. Diets rich in conjugated linoleic acid and vaccenic acid have no effect on blood pressure and isobaric arterial elasticity in healthy young men. J Nutr. 2006;136:992–7.
Pfeuffer M, Fielitz K, Laue C, Winkler P, Rubin D, Helwig U, et al. CLA does not impair endothelial function and decreases body weight as compared with safflower oil in overweight and obese male subjects. J Am Coll Nutr. 2011;30:19–28.
• Bähr M, Fechner A, Kiehntopf M, Jahreis G. Consuming a mixed diet enriched with lupin protein beneficially affects plasma lipids in hypercholesterolemic subjects: a randomized controlled trial. Clin Nutr. 2015;34:7–14. In this crossover study, the dietary supplementation with 25 g/day of lupin protein reduced significantly plasma levels of total, LDL, and HDL cholesterol, triglycerides, and uric acid.
Marchesi M, Parolini C, Diani E, Rigamonti E, Cornelli L, Arnoldi A, et al. Hypolipidaemic and anti-atherosclerotic effects of lupin proteins in a rabbit model. Br J Nutr. 2008;100:707–10.
Pilvi TK, Jauhiainen T, Cheng ZJ, Mervaala EM, Vapaatalo H, Korpela R. Lupin protein attenuates the development of hypertension and normalises the vascular function of NaCl-loaded Goto-Kakizaki rats. J Physiol Pharmacol. 2006;57:167–76.
•• Pirro M, Mannarino MR, Bianconi V, Simental-Mendía LE, Bagaglia F, Mannarino E, et al. The effects of a nutraceutical combination on plasma lipids and glucose: a systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2016;110:76–88. In this meta-analysis of 14 randomized clinical trials enrolling 1670 patients, oral supplementation with a nutraceutical combination containing red yeast rice, berberine, policosanol, astaxanthin, coenzyme Q10, and folic acid was associated with a significant reduction of plasma levels of total cholesterol, LDL cholesterol, HDL cholesterol, triglycerides, and glucose; the improvement of lipid profile was not associated with the duration of supplementation nor with the baseline lipid levels.
• Spigoni V, Aldigeri R, Antonini M, Micheli MM, Fantuzzi F, Fratter A, Pellizzato M, Derlindati E, Zavaroni I, Bonadonna RC, Dei Cas A. Effects of a new nutraceutical formulation (berberine, red yeast rice and chitosan) on non-HDL cholesterol levels in individuals with dyslipidemia: results from a randomized, double blind, placebo-controlled study. Int J Mol Sci. 2017;18:1498. In this double-blind, placebo-controlled, randomized clinical trial, a nutraceutical combination containing berberine 200 mg, monacolin K 3 mg, chitosan 10 mg, and coenzyme Q 10 mg reduced significantly plasma non-HDL cholesterol, LDL cholesterol, and apolipoprotein B levels.
• Cicero AFG, Fogacci F, Bove M, Veronesi M, Rizzo M, Giovannini M, et al. Short-term effects of a combined nutraceutical on lipid level, fatty liver biomarkers, hemodynamic parameters, and estimated cardiovascular disease risk: a double-blind, placebo-controlled randomized clinical trial. Adv Ther. 2017;34:1966–75. In this double-blind, placebo-controlled, randomized clinical trial, a nutraceutical combination containing red yeast rice (10 mg), phytosterols (800 mg), and L-tyrosol (5 mg) reduced significantly total cholesterol, LDL cholesterol, hepatic steatosis index, and systolic blood pressure and improved significantly endothelial reactivity and estimated 10-year cardiovascular risk score compared to placebo.
Cicero AF, Colletti A, Rosticci M, Grandi E, Borghi C. Efficacy and tolerability of a combined lipid-lowering nutraceutical on cholesterolemia, hs-CRP level and endothelial function in moderately hypercholesterolemic subjects. J Biol Regul Homeost Agents. 2016;30:593–8.
• Cicero AF, Morbini M, Rosticci M, D”Addato S, Grandi E, Borghi C. Middle-term dietary supplementation with red yeast rice plus coenzyme Q10 improves lipid pattern, endothelial reactivity and arterial stiffness in moderately hypercholesterolemic subjects. Ann Nutr Metab. 2016;68:213–9. In this double blind, placebo-controlled, randomized clinical trial, oral supplementation with monacolins 10 mg and coenzyme Q10 30 mg reduced significantly plasma LDL cholesterol levels and improved significantly endothelial reactivity and arterial stiffness compared to placebo.
• Pirro M, Mannarino MR, Ministrini S, Fallarino F, Lupattelli G, Bianconi V, et al. Effects of a nutraceutical combination on lipids, inflammation and endothelial integrity in patients with subclinical inflammation: a randomized clinical trial. Sci Rep. 2016;6:23587. In this randomized, open-label, interventional study, oral supplementation with a nutraceutical combination containing policosanol, red yeast rice, berberine, astaxanthin, folic acid, and coenzyme Q10 reduced significantly plasma total cholesterol, LDL cholesterol, and hs-CRP levels and circulating endothelial microparticle levels compared to no active treatment.
• Cicero AF, Morbini M, Parini A, Urso R, Rosticci M, Grandi E, et al. Effect of red yeast rice combined with antioxidants on lipid pattern, hs-CRP level, and endothelial function in moderately hypercholesterolemic subjects. Ther Clin Risk Manag. 2016;12:281–6. In this crossover study, oral supplementation with monacolins 10 mg combined with anti-oxidants was followed by a greater percentage change in plasma total, LDL, and non-HDC cholesterol, hs-CRP, and endothelial function compared to placebo.
• Trimarco V, Izzo R, Stabile E, Rozza F, Santoro M, Manzi MV, et al. Effects of a new combination of nutraceuticals with Morus alba on lipid profile, insulin sensitivity and endotelial function in dyslipidemic subjects. A cross-over, randomized, double-blind trial. High Blood Press Cardiovasc Prev. 2015;22:149–54. In this crossover study, a nutraceutical combination containing red yeast rice (monacolin K 3.3 mg), berberine 531.25 mg, and leaf extract of Morus alba reduced significantly plasma levels of triglycerides, total and LDL cholesterol, glycated hemoglobin, fasting glucose, insulin plasma levels, and HOMA index and increased significantly plasma HDL cholesterol levels; the impact on total and LDL cholesterol reduction was more pronounced than that of a nutraceutical combination containing policosanol, red yeast rice (monacolin K 3 mg), berberine 500 mg, astaxanthin, folic acid, and coenzyme Q10.
Derosa G, Bonaventura A, Bianchi L, Romano D, D'Angelo A, Fogari E, et al. A randomized, placebo-controlled study on the effects of a nutraceutical combination of red yeast rice, silybum marianum and octasonol on lipid profile, endothelial and inflammatory parameters. J Biol Regul Homeost Agents. 2014;28:317–24.
Affuso F, Ruvolo A, Micillo F, Saccà L, Fazio S. Effects of a nutraceutical combination (berberine, red yeast rice and policosanols) on lipid levels and endothelial function randomized, double-blind, placebo-controlled study. Nutr Metab Cardiovasc Dis. 2010;20:656–61.
Affuso F, Mercurio V, Ruvolo A, Pirozzi C, Micillo F, Carlomagno G, et al. A nutraceutical combination improve World J Cardiol s insulin sensitivity in patients with metabolic syndrome. 2012;4:77–83.
Pirro M, Lupattelli G, Del Giorno R, Schillaci G, Berisha S, Mannarino MR, et al. Nutraceutical combination (red yeast rice, berberine and policosanols) improves aortic stiffness in low-moderate risk hypercholesterolemic patients. PharmaNutrition. 2013;1:73–7.
Schillaci G, Pirro M, Ronti T, Gemelli F, Pucci G, Innocente S, et al. Prognostic impact of prolonged ventricular repolarization in hypertension. Arch Intern Med. 2006;166:909–13.
St-Pierre AC, Bergeron J, Pirro M, Cantin B, Dagenais GR, Després JP, et al. Effect of plasma C-reactive protein levels in modulating the risk of coronary heart disease associated with small, dense, low-density lipoproteins in men (The Quebec Cardiovascular Study). Am J Cardiol. 2003;91:555–8.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387–97.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Vanessa Bianconi, Massimo Raffaele Mannarino, Amirhossein Sahebkar, Teresa Cosentino, and Matteo Pirro declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Lipid Abnormalities and Cardiovascular Prevention
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Bianconi, V., Mannarino, M.R., Sahebkar, A. et al. Cholesterol-Lowering Nutraceuticals Affecting Vascular Function and Cardiovascular Disease Risk. Curr Cardiol Rep 20, 53 (2018). https://doi.org/10.1007/s11886-018-0994-7
Published:
DOI: https://doi.org/10.1007/s11886-018-0994-7