Abstract
Context: It is well established in the literature that healthier diets cost more than unhealthy diets. Objective: The aim of this review was to examine the contribution of food prices and diet cost to socioeconomic inequalities in diet quality. Data Sources: A systematic literature search of the PubMed, Google Scholar, and Web of Science databases was performed. Study Selection: Publications linking food prices, dietary quality, and socioeconomic status were selected. Data Extraction: Where possible, review conclusions were illustrated using a French national database of commonly consumed foods and their mean retail prices. Data Synthesis: Foods of lower nutritional value and lower-quality diets generally cost less per calorie and tended to be selected by groups of lower socioeconomic status. A number of nutrient-dense foods were available at low cost but were not always palatable or culturally acceptable to the low-income consumer. Acceptable healthier diets were uniformly associated with higher costs. Food budgets in poverty were insufficient to ensure optimum diets. Conclusions: Socioeconomic disparities in diet quality may be explained by the higher cost of healthy diets. Identifying food patterns that are nutrient rich, affordable, and appealing should be a priority to fight social inequalities in nutrition and health.
Keywords: diet cost, energy density, food prices, nutrient density, nutrition economics, socioeconomic status
INTRODUCTION
The argument that food costs influence diet quality and so contribute to the observed social inequalities in health is not new.1 The classic 1936 work of John Boyd Orr, Food, Health and Income,2 documented the existence of a social gradient in diets and health in Depression-era Great Britain. At the time, the method of grouping the population according to per capita incomes was new and open to criticism. George Orwell3 also commented on the dismal diets of the British working poor. Then, as now, lower-income groups had cheaper but lower-quality diets and worse health outcomes as compared with the rich.
The low cost of calories from added sugars and fats in relation to diets and health was also noted by James et al.1 The argument was that food and nutrition played a key part in social inequalities in health, with poor health resulting from buying “foods richer in energy (high in fat and sugar) to satisfy hunger, which are much cheaper per unit of energy than foods rich in protective nutrients (like fruits and vegetables).”1 The social disparities in diet and health, observed in Britain at the time, were said to be widening.1 According to very recent data from the United States,4 they are continuing to grow.
Studies on the social gradient in obesity rates also concluded that “the association between poverty and obesity may be mediated, in part, by the low cost of energy-dense foods and may be reinforced by the high palatability of sugar and fat.”5 It was noted that the good-tasting fats and sweets6 were also easy to consume in excess.7,8 Their palatability, availability, and convenience9,10 made low-cost calories the likely direct precursors of weight gain.11,12
This pattern of social inequalities in diet quality and health continues to be observed in most industrialized countries, including the United Kingdom,13 France,14,15 Finland,16 Belgium,17 Ireland,18 Australia,19 and the United States.20,21 However, the published evidence on the relation between diet quality and socioeconomic status has been based largely on associations found in cross-sectional studies. Although such studies can be used to generate hypotheses, they do not prove causality. In particular, such associations do not permit the conclusion that lower incomes and limited food budgets are the primary cause of unhealthy food choices.
In the absence of longitudinal cohort studies, the modeling of French food patterns has provided new insights into how a constraint on diet cost can have a negative impact on diet quality.22,23. Notably, imposing a sharp limit on diet costs invariably led to modeled food patterns that were energy dense but nutrient poor and were similar in composition to diets consumed by lower-income groups.22,23 It is worth noting that an inadvertent confirmation of French modeling studies was provided by recent economic analyses of empirical data from the United Kingdom.24 In the wake of the economic recession of 2008, more British consumers have turned to foods with lower cost per calorie, that is, to more energy-dense foods that are higher in sugars and fats and lower in nutritional value.24
That healthier diets cost more than unhealthy diets is well established in the literature.25–37 The present systematic review provides evidence to support two additional points: the low cost of empty calories relative to the higher cost of nutrient-rich foods may partly explain the observed social inequalities in diets and health,38,39 and food budgets of lower-income groups are insufficient to assure access to a healthy diet.
METHODS
The goal of this systematic literature review was twofold: to examine whether nutrient-rich foods and higher-quality diets in different societies generally cost more, and to discuss food prices in relation to the diet quality of lower–socioeconomic status groups on the basis of data from multiple countries. This review followed the meta-analysis of observational studies in epidemiology (MOOSE) guidelines for systematic reviews. The criteria used to define the research question are presented in Table 1, using an adapted problem, intervention, comparison, outcomes, and setting (PICOS) strategy. The principal conclusions, based on the literature review, were illustrated further using a national French database listing the nutrient composition of commonly consumed foods and their mean retail prices.
Table 1.
Description of the PICOS criteria used to define the research question
| Parameter | Description |
|---|---|
| Population | Inclusion: presumably healthy adults |
| Exclusion: none | |
| Intervention/correlate | Inclusion: economic and financial correlates, nutrition economics, diet cost, sociodemographics |
| Exclusion: none | |
| Comparison | Not applicable, since observational studies and correlations rather than interventions were reviewed |
| Outcome | Inclusion: nutritional quality, cost, dietary patterns, along with data on social disparities and inequality |
| Exclusion: none | |
| Study design | Inclusion: studies describing the monetary cost and nutritional quality of food and diets in relation to social disparities, poverty, or food insecurity |
| Exclusion: letters, editorials, commentaries, studies published prior to the year 2000 |
Literature search strategy
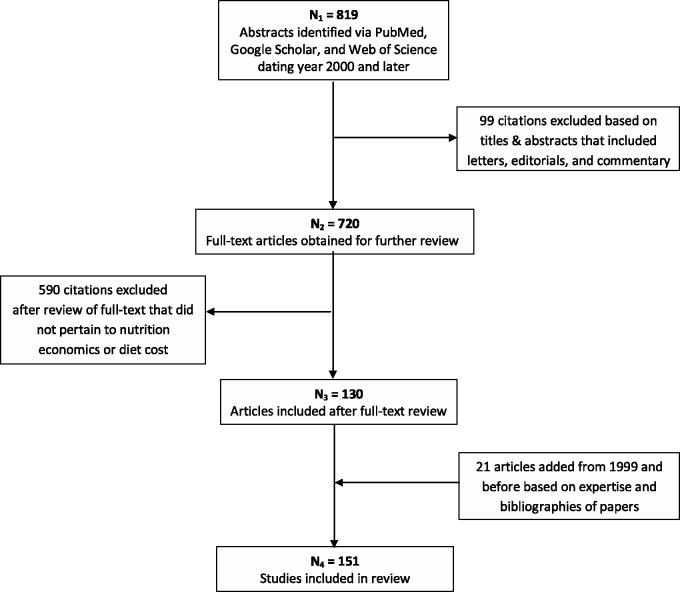
The search, conducted in 2014 using PubMed, Google Scholar, and Web of Science databases, identified publications linking food prices, dietary quality, and socioeconomic status. As shown in Figure 1, the literature search led to 819 abstracts dating to the year 2000 and later. Letters, editorials, and commentaries were excluded on the basis of titles and abstracts, leading to 720 full-text articles. The list was further restricted to 130 articles after 590 citations that did not pertain to nutrition economics or diet cost were excluded after review of the full text. Twenty-one articles dating prior to the year 2000 were included in the review on the basis of expert consultations and bibliographies of papers published by researchers, including the present authors. These processes yielded the 151 studies on diet cost and nutrition economics that formed the basis of the present review.
Figure 1.
Flowchart of search and screening process for studies on nutrition economics and diet cost
Data analysis
To confirm conclusions from the literature, the relations between the nutritional quality of food and the price of food were assessed using a French nutrient composition table for 1117 food items consumed by a representative sample of 2624 adults participating in the 2006–2007 national dietary survey INCA2.40 The national food price database for France was obtained from the 2006 Kantar Worldpanel, based on annual food expenditures of a representative sample of 12 000 French households. For each food item reported as consumed by INCA2 respondents, its standard price was calculated by dividing the annual expenditures by the amounts purchased for all the food products corresponding to this item in the Kantar Worldpanel and available on the French market. Given that these prices were paid by a representative panel of consumers, the standard prices were weighted by the most frequently purchased forms of each food. After adjusting for preparation and waste, food prices in the database were expressed in euros per 100 g of edible portion. Median and mean costs of energy (i.e., energy cost in €/100 kcal) provided by foods were calculated for each main food group. Nutrient quality of foods was estimated using the SAIN:LIM ([score of nutritional adequacy of individual foods] ÷ [score of nutrient to be limited]) ratio, calculated as described.41,42 Correlation analyses were conducted to assess the relation between energy density (kcal/100 g) and energy cost and between nutrient quality and energy cost.
RESULTS AND DISCUSSION
Relation between food prices and adoption of healthier diets by lower-income groups
That food prices have a disproportionate impact on lower-income households is a direct consequence of Engel’s Law.43 As incomes rise, the absolute amount of money spent on food increases, but the proportion of income spent on food drops.43 Whereas average food spending in the United States has been estimated at around 11% of income, households in poverty can spend more than 25%.5 As a result, the impact of food prices on dietary choices in the United States tends to be underestimated by higher–socioeconomic status groups that are affected the least.44,45 In France, households in the top decile of incomes spent 22% of disposable income on food in 2006, whereas those in the bottom decile spent as much as 29%.46
In surveys on motivations for purchases, consumers indicate that, along with taste and convenience, the price of food is one of the main factors influencing their food choices. This is especially true for lower-income households.47,48 Multiple socioanthropological studies have shown that food prices weigh more heavily on purchase decisions made by lower-income groups.49–51
Repeatedly, lower-income respondents have identified economic factors as the main barriers to adopting healthier diets. The high perceived cost of fruit and vegetables was noted,52 as was the high price of meat, perceived as an integral part of the core diet.51,53 Although lower-income groups did not purchase less meat, they bought cheaper and fattier cuts.46,49,54 Poor women in Australia, when asked what foods they would include in the market basket if given another 25% to spend, selected foods of higher nutritional value.55
In focus groups, low-income women in the United Kingdom53 and in Holland56 have likewise stressed the key role of food prices. Foods reputed to be unhealthy were considered to be cheaper than healthier foods. They were easier to find and to prepare, and children preferred them because they were tastier. Low-income mothers in St Paul, Minnesota, reported in focus groups that they knew fruit and vegetables were healthy and that they would like to eat them more often and give them to their children, but that they could not afford to do so.57 Similarly, participants in a qualitative survey in Paris58 recognized vegetables, fruit, dairy products, fish, and fresh produce as “healthy,” and said that they would buy them more often if only they had the means. Perceived as a dietary priority for children, dairy products were viewed as affordable, unlike fish, fresh vegetables, or fruit.58 These families' diets were monotonous, which is partly explained by the reluctance to try new foods, given the potential risk of food waste, which is an intolerable situation in poverty.58
In the United States, the observed links between socioeconomic status and diet quality were partly explained by the perceived importance of food prices.59 Among lower-income groups, a perception of food price as very important was linked to more energy-dense diets.60 By contrast, the perceived importance of good nutrition did not differ by socioeconomic status.60 Having positive attitudes toward nutrition did not remove the critical influence of socioeconomic status on diet quality.61
Merging food prices with nutrient composition data
Self-reports by lower-income groups, as reported in the literature, suggest but do not prove that the social gradient in diet quality is partly caused by higher prices of more nutrient-rich foods. Researchers studying the nutrient density of foods in relation to their monetary cost need access to detailed data on food nutrient composition and price. It was not until the late 1990s that data on the nutritional composition of food products were introduced into surveys on food purchases62 and – conversely – data on food prices were introduced into surveys on food consumption.63 In 1994, Australian researchers estimated the price of each of the 229 foods on the frequency questionnaire used in a food survey of the general population25 using supermarket food prices. Since that time, retail food prices have been obtained for research purposes from a variety of sources, both public and private.26,29,31–33,35,64–67 In general, food prices were incorporated as a vector in the nutrient composition database and were treated as an additional “nutrient.”
Both France and the United States have national food price databases that are available for research purposes. The French database, based on purchase data from the Secodip panel (later called the Nielsen and then the Kantar Worldpanel), was compiled in 1997 to analyze diet costs in the national INCA1 dietary survey.29,64 An updated Kantar food price database created in 2007 was merged with the INCA2 nutrient composition data to generate the illustrative tables and figures for the present review.
The US Department of Agriculture’s national food price database,68 which corresponds to the National Health and Nutrition Examination Survey (NHANES) 2001–2002 data, was released in 2008. Other than one update for 2003–2004 NHANES, no further updates have been released. However, that database was sufficient to link national food prices in the United States with the NHANES food recalls35 and with food frequency questionnaires.33,35 Other researchers obtained prices from the National Food Survey in the United Kingdom26 or the Department of Trade and Tourism in Spain.31,32
Food prices were also obtained from supermarkets and the Internet,37,65,67 or directly from a distributor.66 When the prices were from supermarkets or the Internet, researchers developed pricing protocols, selecting multiple items or lower-cost foods in family-sized packaging.65,67 When the prices were drawn from surveys on food expenditures, the average price paid (mean price weighted by the quantities bought) was calculated.68,69 For example, the average price of green beans reflected the price of fresh, canned, and frozen green beans of several brands, weighted by the quantities consumed by the population.29 Supermarket data have been used to assess the energy cost and nutrient content of a freely chosen market basket of foods.70
In all cases, fresh foods as purchased were then transformed into edible foods as consumed, adjusting for preparation and waste. Since cooked pasta absorbs water, 100 g of cooked pasta costs 3 times less than 100 g of dry pasta. Since banana peel is discarded, 100 g of peeled banana costs 1.3 times more than 100 g of fresh banana with skin. For research purposes, all food prices were converted into values per 100 g of edible portion and were merged with the nutrient composition data.
Estimating the monetary cost of diets using retail prices, whether local or national, does not always take temporal trends in diets or health into account. For example, a decline in food prices has been linked to higher obesity rates in the United States.71,72 In reality, only the price of energy-dense foods73 and sweetened beverages74 has declined, whereas the prices of fresh vegetables and fruit and low-fat dairy continue to climb.73,75,76 In France, the prices for vegetables have risen steeply, whereas the prices for dietary fats have dropped.77 One study used correction factors based on a consumer price index to estimate the differential in food prices between the time of price collection and the time at which the dietary data were collected.78
Lower cost of energy-dense foods
Comparative metrics of food cost have been based on energy and nutrient content expressed per 100 g of edible portion.69 Table 2 shows the energy density (in kcal/100 g), the price (€/100g), and the energy cost (€/100 kcal) of several foods, as based on the INCA2 nutrient composition food database and 2007 prices of current food items, ranked by decreasing order of energy cost. Potato chips, sweets, and biscuits (cookies) were more expensive in terms of euros per kilogram than were low-energy-density apples, tomatoes, and carrots but were cheaper in terms of euros per 100 kcal. This is because apples, tomatoes, and carrots have a higher water content than do sweets and fats. As noted by Atwater in 1896,79 water in foods drives energy density because it provides bulk but no energy or nutrients. Given the economic importance of obtaining 2000 kcal per day at an affordable cost, the preferred method of comparing food prices has been per calorie, as opposed to per serving or per unit weight.79,80
Table 2.
Energy value, purchase price, and cost of energy for selected food items in France
| Food item | Energy value, in kcal/100 g | Purchase price, in €/100 g (edible part) | Cost of energy, in €/100 kcal |
|---|---|---|---|
| Sunflower oil | 900 | 0.13 | 0.01 |
| Pasta, cooked | 115 | 0.05 | 0.04 |
| White bread, sliced | 281 | 0.21 | 0.07 |
| Biscuits (cookies) | 484 | 0.56 | 0.11 |
| Sweets | 450 | 0.60 | 0.13 |
| Potato chips | 504 | 0.84 | 0.16 |
| Whole-meal bread | 269 | 0.45 | 0.17 |
| Pâté | 410 | 0.85 | 0.21 |
| Cola soft drink | 41 | 0.09 | 0.22 |
| Ground beef, 15% fat | 239 | 0.67 | 0.28 |
| Orange juicea | 44 | 0.14 | 0.32 |
| Yogurt | 47 | 0.18 | 0.38 |
| Apples, fresh | 45 | 0.18 | 0.39 |
| Almonds | 634 | 2.51 | 0.41 |
| Carrots, fresh | 32 | 0.14 | 0.44 |
| Ground beef, 5% fat | 121 | 1.10 | 0.91 |
| Tomatoes, fresh | 20 | 0.28 | 1.39 |
| Cod, frozen | 94 | 1.95 | 2.07 |
| Lettuce, fresh | 14 | 0.32 | 2.28 |
| Strawberries, fresh | 28 | 0.80 | 2.85 |
aFrom concentrate.
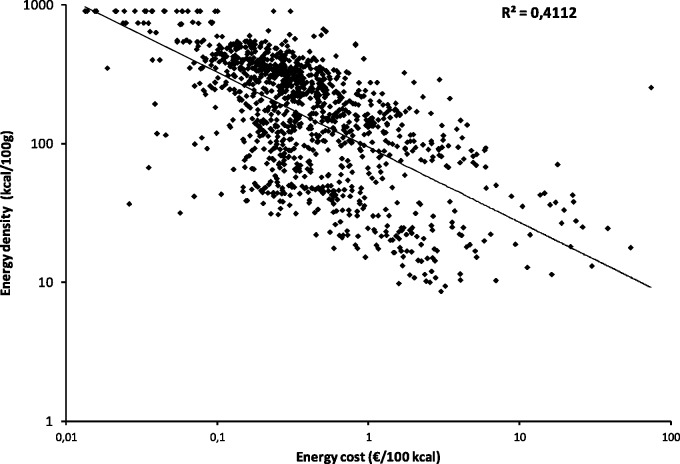
In general, grains, fats, and sweets were associated with lower per-calorie food costs (energy cost, in €/100 kcal). By contrast, fruits and vegetables were associated with higher per-calorie food costs. As a result, the relation between the energy density of foods and the energy cost was negative.27,28,66,81 Figure 2 shows the negative relation between energy density and energy cost of foods, based on 2007 food prices in France.
Figure 2.
Energy density (kcal/100 g) and energy cost (€/100 kcal) of foods (n = 1117) in the French food database, based on 2007 national food prices
The results confirm previous findings obtained with 1997 food prices,30,69 with energy-dense foods such as fats and oils, added sugars, and refined grains providing calories at the lowest cost, while low-energy-density lean meats, fish, vegetables, and fruit are the most expensive energy sources. Similar findings have been obtained in the United States,79,82 Australia,81 and the Netherlands.66 The inverse relation between energy density of foods and their energy cost held both between and within food groups.83
Higher cost of nutrient-rich foods
Studies on the relative cost of energy-dense compared with nutrient-dense foods critically depend on accurate metrics of nutrient density. In the past, the relative healthiness of different foods was based on the most arbitrary of criteria.5 More recently, the nutritional value of different foods was established using more objective nutrient profiling techniques.30,69,83
Foods can be ranked or rated on the basis of their nutrient content relative to calories. Typically, nutrient profile models represent the ratio of nutrients to calories. One nutrient profiling model, the French SAIN,LIM nutrient profiling system, is based on two scores: SAIN, the score of nutritional adequacy of individual foods, and LIM, the score of nutrient to be limited.41 Whereas SAIN is based on beneficial nutrients (protein, fiber, vitamins, and minerals) whose intake is to be encouraged, LIM measures the content of nutrients to be limited: saturated fat, added sugar, and sodium. In published studies, foods were divided into four categories on the basis of their relative SAIN and LIM scores.41 Overall nutritional quality of foods was also estimated by the SAIN:LIM ratio.42 Importantly, the concept of nutrient density was clearly distinguished from the energy density of foods.82
The US-based Nutrient Rich Foods Index calculated the nutrient content of foods, expressed as the percent daily value per 100 kcal.84,85 The Nutrient Rich Foods Index was based on 9 nutrients to encourage – protein; fiber; vitamins A, C, and E; calcium; iron; magnesium; and potassium – and on 3 nutrients to limit – saturated fat, added sugar, and sodium. The final algorithm was the sum of percent daily values for the 9 positive nutrients minus the sum of percent daily values for the 3 nutrients of public health concern. These two nutrient profiling models have served as the basis of several quantitative studies on the relation between the nutritional quality of foods and their cost.30,42,69,83
Multiple studies based on French food databases have shown that higher nutrient density scores were directly linked to higher per-calorie cost.30,69 In general, the more nutrient-rich foods were more expensive per kilocalorie than were foods of lower nutritional value.86 However, there was a wide variability in nutrient density and cost within food groups.30 For example, not all vegetables were equally expensive. The question of concern was which vegetables, including juices and soups, provided the most nutrients per unit cost.87 Nutrient density was measured using the Nutrient Rich Foods Index, and food cost was calculated per 100 g, per 100 kcal, and per serving. Analyses showed that tomato juices and tomato soups, dark green leafy and nonleafy vegetables, and deep yellow vegetables, including sweet potatoes, had the highest Nutrient Rich Foods Index scores overall. Highest Nutrient Rich Foods Index scores per dollar were obtained for potatoes, tomato juices and tomato soups, carrots, and broccoli. Processed vegetables, soups, and juices providing affordable nutrition87 are often the choices reported by groups of lower socioeconomic status.39
Estimating monetary cost of individual-level diets
The ability to estimate diet costs is a prerequisite for studies on the relation between socioeconomic status, diet quality, and health.88 The collection of such data, however, has been hampered by methodological problems. First, dietary and economic data at the national level tend to be collected by different agencies. In the United States, the NHANES, the basis for many policy decisions, provides no data on food prices or food expenditures.35 Conversely, surveys of food expenditures collected by the US Bureau of Labor Statistics lack data on food consumption or health and are collected at the level of the household.
Studies in nutritional epidemiology that use individual health outcomes require that all dietary variables be at the individual level. Data collected at different levels of aggregation pose problems for any analyses of diets and health. In particular, household food expenditures are difficult to link to individual health outcomes. One approach to studying the relation between diet quality and diet cost, adopted early by the present authors, was to attach standard food prices or individual food expenditures to dietary intake data.88
Following the design of classic intermethod validity studies,89–91 Monsivais et al.92 compared three alternative methods of estimating individual diet costs. First, 4-day food diaries were linked with actual food expenditures as documented by store receipts. Second, 4-day food diaries were linked to local supermarket food prices. Third, food frequency questionnaire data were linked to local food prices. Attaching supermarket prices to dietary intake data allowed the calculation of the intrinsic monetary cost of each study participant’s diet.92 All three estimates of diet cost were significantly linked to household incomes.92 Another study also compared the estimated diet cost with either true expenditures (grocery receipts) or a vector of standard food prices.78 The results showed that the mean diet cost estimates for the whole population were similar with the two methods, but that at the individual level, estimates differed by as much as £3.00/d.78 Another study also found relatively weak agreement between diet costs estimated with standard prices and with prices actually paid by individuals.93
Although the expenditure-based method might be thought to be the true indication of diet cost, it had no parallel in nutritional epidemiology studies. Dietary surveys do not estimate the nutrient value of each food as consumed by each study participant. Instead, researchers have estimated individual energy and nutrient intakes on the basis of standard nutrient composition tables. For example, the vitamin C content of fresh, raw apples, as consumed by NHANES participants, has been set at 4.6 mg per 100 g of edible portion in the Food and Nutrient Database for Dietary Studies nutrient composition database.94 That estimate may or may not accurately reflect the vitamin C content of the apples that the NHANES participants had actually consumed. In the studies described below, a cost vector (i.e., standard food prices) was inserted into the nutrient composition database.
The key to modeling individual diet costs is to treat the monetary cost variable as analogous to a nutrient variable.26 Individual daily diet costs are then estimated by attaching dietary intakes to national or local food prices.25–29,31–35,37,64–67,95–100 In epidemiologic studies, an adjustment for energy content is made to test the relation between a given nutrient and the outcome variable of interest.101,102 Similarly, in most of the studies described below, an adjustment for energy was made to test the relation between diet cost and the outcome variables of interest and to allow for comparisons across population subgroups.
This method of estimating individual diet costs on the basis of prevailing retail prices makes the strong assumption that foods are purchased at retail and prepared and eaten at home. Such an assumption may well underestimate the real variability of food prices and of the costs associated with individual food consumption. Food cost variations that may be attributable to home preparation of certain foods, purchase of away-from-home foods, differences between brand foods and generic or low-cost foods, or differences between out-of-season and in-season foods are overlooked with the use of the average price. However, the exact same caveats apply to the average content of calories, fiber, vitamins, and minerals of foods. Nutrient composition data sets have been based on many of the same assumptions.
In general, researchers have treated food prices per 100 g of edible portion as equivalent to a nutrient composition vector and have integrated food prices into the nutrient composition database. That nutrient composition database was then used to estimate individual-level energy and nutrient intakes and individual-level diet cost on the basis of dietary intake data obtained using different methods. In published studies, standard food prices were linked with dietary intakes obtained using food frequency instruments or food frequency questionnaires.26,31,33,34,37,65,96–98,103 However, standard prices were also attached to data from diet records,29,64 dietary history,27,28 or 24-hour recalls.15,66
Do healthier diets cost more?
The earliest studies on the higher cost of healthier diets were conducted in Australia and the United Kingdom.25,26,104 Although rarely cited, those studies were among the first to model the cost of the recommended diets. Cade and Booth104 attached supermarket food prices to dietary intake data in the United Kingdom to compare the relative cost of healthy and less-healthy diets. Diets consistent with a set of 6 nutritional guidelines cost 10% more, although the difference was not statistically significant.104 McAllister et al.25 attached supermarket prices to 229 foods to compare the costs of observed and recommended diets. The recommended diets provided 15% less energy, meaning that the energy-adjusted cost of healthier diets was higher.
The linear relation between diet quality and cost was shown, for the first time, in the 1999 study of diets of more than 15 000 women in the UK Women’s Cohort Study.26 As diet quality, measured by the Healthy Diet Index, increased, so did the estimated daily amount spent on food. This relation persisted after adjusting for energy intakes. The Healthy Diet Index was based on saturated fatty acids, polyunsaturated fatty acids, proteins, carbohydrates, free sugars, and fibers and on two food groups (fruit and vegetables, and pulses, grains, and nuts). The positive relation between diet quality and cost was recently confirmed in the same cohort of women.37 The dietary pattern that was most in accordance with the UK EatWell Plate guidelines cost twice the price of the least-healthy diet (£6.63/d vs £3.29/d) and was consumed by women with higher education level and higher occupation status.37 A recent meta-analysis of food prices collected after year 2000 found a smaller difference of US $1.5 (average for 10 different countries) between the healthiest dietary patterns and the least healthy ones.36
Healthier diets were also found to cost more using food- and nutrient-based measures of diet quality, such as the Mediterranean Diet Score,99,105 the Healthy Eating Index,99,100,105 the Dietary Approaches to Stop Hypertension score,106 and the modified Healthy Eating Index.33,35 A positive association was also observed between diet cost and dietary diversity,37,100 and between diet cost and nutrient-based scores, whether nutrients were computed separately29,32,34,65,67,107,108 or aggregated into a composite measure such as the Mean Adequacy Ratio.30,103 In some studies, data-driven dietary patterns (e.g., derived by cluster analysis) were scored according to how well they complied with a specific desirable food pattern.37,95
Dietary energy density27 has also been used as a measure of diet quality. Attaching 50 food prices to the dietary survey data from the Val de Marne study27,28 showed that energy-dense diets were associated with lower diet costs.27 By contrast, higher-quality diets were associated with higher energy-adjusted diet costs.
Similar results were obtained using the nationally representative INCA1 dietary survey and the retail prices for over 800 foods in France, based on purchase data from Secodip, a nationally representative panel of consumers.29,64 Importantly, lower dietary energy density and higher nutrient content were each independently associated with higher energy-adjusted diet costs.64 When dietary intakes data from two different populations in Spain were examined, the same direct correlation between diet quality and cost was found.31,32,95 Similar results were later reported in a representative sample of adults in Greece99 and in two cohorts of young adults and of elderly persons in Holland.66 In the United States, the same correlations were found using food prices attached to data from diet records65,96 and from food frequency questionnaires.34,67,103,107
Most of the evidence on the relation between diet quality and diet cost was provided by cross-sectional studies, many based on samples of convenience. At least two sets of studies were based on nationally representative population samples in France29,64 and in the United States.35 Only one US study estimated the diet costs of a nationally representative sample of adults in the NHANES 2001–2002 study.35 In that study, higher values of the Healthy Eating Index were linked to higher diet costs and higher respondent socioeconomic status.35
In multiple studies, specific food and nutrient intakes were associated with lower energy-adjusted diet costs. First, the consumption of energy-dense foods (kcal/100 g) was associated with lower diet costs per 100 kcal.27,65,66,96 Second, higher consumption of added sugars and saturated and trans fats was also associated with lower diet costs.28,35,65,67 Sodium content of the diet was not systematically linked to energy costs.35,108
The same associations between diet quality and cost held across different countries, across different age groups, and for different indicators of diet quality. Only one study conducted in Japan drew slightly different conclusions. Consistent with other findings, higher energy cost was linked to lower energy density. However, higher diet costs were linked to higher consumption of cholesterol and total and saturated fats,108 which was not the case in either the United States35 or France.29 The Japanese study108 was conducted with dietetics students whose fat consumption was far below international norms. The Japanese study also differed because the typical food consumed in Japan was different than that consumed in other countries included in this review.
Relation between different food groups and diet cost
Vegetables and fruit, recognized as the core components of a healthy diet, also account for a large part of diet cost. In the pioneering Cade et al.26 study, fruits and vegetables drove the diet quality score and also accounted for the biggest share of the total diet cost. The observation that diets high in fruits and vegetables had highest per-calorie diet costs was subsequently confirmed in Spain,31 Greece,99 the United States,35 and Sweden.100 In Japan, the highest proportion of diet cost was attributable to fish and vegetables.98 Among low income women in California, greater vegetable variety was associated with higher Healthy Eating Index scores and lower dietary energy density, but also with higher diet costs.109
In the average French diet, the highest proportion of diet cost was attributable to meat, fish, vegetables, and fruit.27,28 These food groups account for a far smaller proportion of energy intakes. By contrast, starches, added fats, and fatty, sweet, and/or salty products provided a large proportion of energy, while contributing relatively little to the total cost of food.30 The consumption of milk and milk products was cost neutral.28 On the basis of the French INCA1 survey, the food group of meat/eggs/fish contributed only 18% of daily calories, while accounting for 35% of diet cost. Fruits and vegetables provided 8% of calories, while accounting for 17% of cost. Starches and added fats contributed 23% and 10% of the total energy intake but only 9% and 2% of the total cost, respectively. The energy contribution of dairy products was equivalent to their cost, around 11%.30
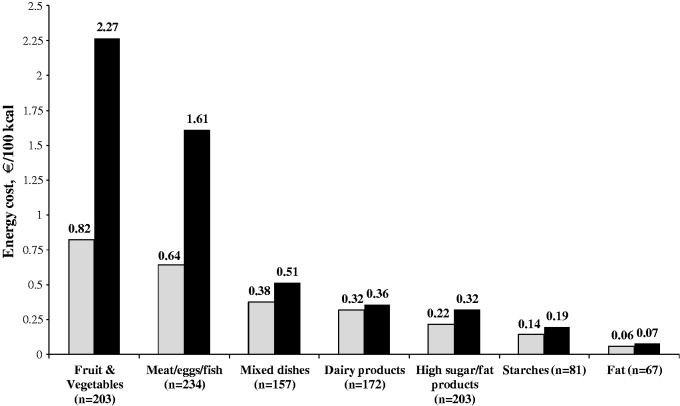
Figure 3, based on the French INCA2 nutrient composition food database and 2007 food prices, indicates the mean and median cost of energy provided by foods in each of the major food groups (€/100 kcal). These results, consistent with those from the INCA1 food survey,30 showed that the fruits and vegetables food group and the meat/eggs/fish group were the most expensive sources of dietary energy. The median cost was €0.82/100 kcal for fruits and vegetables and €0.64/100 kcal for meat/eggs/fish. Dairy products had an intermediate energy cost (€0.32/100 kcal). Fats and sweets only cost €0.22/100 kcal, and refined starches and added fats provided energy at the lowest cost (€0.14/100 kcal and €0.06/100 kcal, respectively).
Figure 3.
Median (in gray) and mean (in black) cost of energy provided by foods in each main food group in the French food database
These illustrative analyses confirmed the major points in the literature. Higher consumption of fruit, vegetables, meat, and fish was associated with higher diet costs. By contrast, higher consumption of fats and oils, added sugars, and refined grains was associated with sharply lower diet costs.28 These analyses essentially confirm the classic 1936 studies of food, health, and incomes in the United Kingdom.2
Modeling dietary choices using linear programming
The question of what combination of foods provides optimal nutrition at the lowest monetary cost can be answered using a diet optimization technique known as linear programming. Initially proposed by Stigler in 1945,110 linear programming was used by Dantzig111 to model optimal food patterns under a variety of constraints.
Linear programming modeling has become the method of choice when it comes to generating food patterns subject to a variety of nutritional, behavioral, and economic constraints.22,23,112,113 Linear programming models have the advantage of being able to isolate economic constraints and examine their impact on food selection. By contrast, empirical data on food choices by the poor can be complicated by a myriad of social, economic, and psychological factors. Linear programming models generally show that budget restrictions have a negative impact on food choices, orienting food patterns toward foods that are both energy dense23 and nutrient poor.22 The US Department of Agriculture’s Thrifty Food Plan, designed to meet dietary guidelines at the lowest possible cost, is a related non–linear programming model.114
In general, linear programming models have tried not to depart too much from the current population diet by introducing new foods that are consumed rarely or not at all.112 The British sociologist Liz Dowler115 has suggested that poor people sought to have the same eating habits as the people around them and not be hungry, rather than meeting nutritional needs at the lowest cost.
Modeling the culturally acceptable choices that people would make without going hungry on an increasingly constrained food budget was the topic of one study.22 The linear programming model removed all the nutritional constraints (except energy) and replaced them with social acceptability constraints, while progressively reducing cost. The resulting food patterns were lower in fruit, vegetables, meat, and fish but sharply higher in fats, sweets, and refined grains. The net result was a rise in energy density and a corresponding decline in nutrient quality of modeled food patterns.22,23 Meat, the lone exception, was not reduced in food patterns of lower-income groups even when it was reduced by the linear programming model.39 Social norms and the symbolic role of meat may ensure that it retains its central role, despite its high cost.51
The food patterns generated by linear programming models were striking similar to those of low–socioeconomic status groups.39 In linear programming models, the selection of food patterns was guided by the necessity to reduce the cost of daily calories and, therefore, by the need to include foods that were inexpensive sources of energy. The observation that the modeled food patterns were of higher energy density suggests a potential link to obesity and weight gain, as hypothesized by the present authors.23 Clearly, one conclusion based on the literature is that many unhealthy food choices associated with poverty may be a direct result of economic constraints. Adopting the recommended diets of lower energy density and higher nutrient content is likely to be associated with higher per-calorie diet costs.116,117
Deliberately selecting an energy-dense diet with no limit on cost,23 however, led to a relatively small decline in diet cost. It would appear that limited food budgets force low-income consumers to select low-cost, low-quality diets, whereas the higher–socioeconomic status groups have the choice of eating well or eating poorly.23 This suggestion is consistent with observations that low-quality diets are not restricted to poor people but are nevertheless more frequent in lower– as opposed to higher–socioeconomic status groups.24,39
Inadequacy of food budgets in poverty
The relation between the cost of healthy food and the household's food budget is of crucial importance. Several studies have compared the price of a balanced market basket of foods to the food budget of poor people in the United Kingdom,118–120 Canada,121,122 Ireland,123 and Australia.124 Based on different populations and different methods, the overall conclusion of those studies was that poor people could not afford a balanced healthy diet.125
In the United Kingdom, Nelson et al.120 concluded that poor people’s food expenditures were below the threshold for a low-cost-but-acceptable market basket of healthy foods. In Ireland, the share of the budget devoted to a balanced diet of “no-brand” foods was estimated at between 40% (for an elderly person living alone) and 80% (for a single-parent household with 1 child) of disposable incomes.123 In Australia, adhering to the national food guidelines would take 40% of income of the poor, defined as those receiving a living allowance from the state, even with a market basket of cheapest or private-label products.124 A 25% budget share was considered acceptable,124 with fruit and vegetables accounting for the largest share of the food budget.124,126 However, in many studies, the definition of a balanced diet was based on experts' guidelines, and the methodology for defining a basket was not described clearly enough to be reproduced. This constitutes a significant limitation.
In France, linear programming modeling was used to generate low-cost nutritionally adequate diets.113 Starting with a dietary intakes database, nutrient adequacy standards, and a list of foods of known nutritional composition and prices, linear programming modeling created food patterns that met nutritional guidelines as well as social acceptability constraints, all at the lowest possible price. The linear programming model was first applied to the Val de Marne data, using 50 food items,127 and later to the INCA1 database, using 614 food items.113 The same theoretical minimal price for a nutritionally adequate diet was obtained from both sets of data, i.e., €3.20/d for women and €3.40/d for men. This amount was about 2 times lower than the average daily food expenditure in France (€6.5/d) but was close to the food budget of people living in poverty.46
Based on the above analyses, the minimum food budget for a nutritionally adequate diet was estimated at €3.5/d. However, that amount imposed significant practical limitations. Even on €3.5/d, the theoretical access to an adequate diet meant zero food waste, drinking water from the tap, knowing how to cook, and not eating out at all. Below that cost level, the linear programming model failed to come up with a mathematical solution. In other words, having a nutritious diet at less than €3.5/d was impossible, not only in practice but also in theory. Yet the average food budget of people receiving food assistance in France was estimated at €2.5/d in 2005,128 well below the theoretical minimum for a nutritionally adequate diet.
In fact, when all consumption and cultural acceptability constraints were removed, it was technically possible to cover an adult’s energy and nutritional needs for under €1.5/d (i.e., 4 times lower than the average expenditure for food in France). However, the food patterns generated were hardly realistic, containing only oil, pasta, potatoes, a little wheat germ, carrots and radishes, milk, liver, and herring.113 Food is not only a matter of nutrition; it is also a marker of cultural and social identity. To be fully effective, dietary recommendations need to be culturally acceptable.
The US Department of Agriculture (USDA) Thrifty Food Plan (TFP) was designed to find foods and combinations of foods that met dietary recommendations, respected the current eating habits of lower-income Americans, and minimized cost.129 The price of TFP market baskets has long served to define the amount of institutional food aid in the United States. The calculated cost of the TFP was between $5.00 and $6.00 per day for adults aged 19–50 years ($37.50 and $42.10 per week for women and men in November 2013). The Economic Research Service of the USDA has estimated mean current food expenditures per capita at $14.00/d.130 Therefore, in line with similar comparisons in France, the minimum cost of a modeled balanced diet and the average expenditure on food varied by more than a factor of 2.
Several authors in the United States have described the TFP amount as insufficient. First, as noted by Wilde and Llobrera,131 the cost of each new revised TFP was not recalculated de novo by taking into account trends in foods habits and food prices; it was simply subtracted from the preceding TFP in order to take inflation into account. Further, prices of food on the TFP menu were underestimated by comparison with real prices.132 The TFP was called unrealistic, not allowing for the growing use of processed, precooked, and away-from-home foods133 or taking into account the time and effort associated with preparing TFP recipes.134
What are affordable acceptable, nutrient-rich foods?
The modeling of French eating habits has shown that low-cost yet nutritious food patterns are theoretically possible, provided that the budget exceeds €3.5/d. However, such optimized food patterns may include foods that are rarely eaten by the general population.113,131 Officially, healthier diets involve increasing the consumption of fruit, vegetables, fish, lean meats, and whole grains, as well as decreasing the intake of animal fats and sweets116; such a pattern was obtained in diets designed to fulfill nutrient recommendations.112 However, cost constraints drove food patterns away from the official dietary guidelines. Although the amount of meat in food patterns was reduced, organ meats and eggs were increased. Furthermore, fresh fruit and dark green vegetables in modeled food patterns were replaced by root vegetables (potatoes, carrots), pulses, nuts, and fruit juices.112
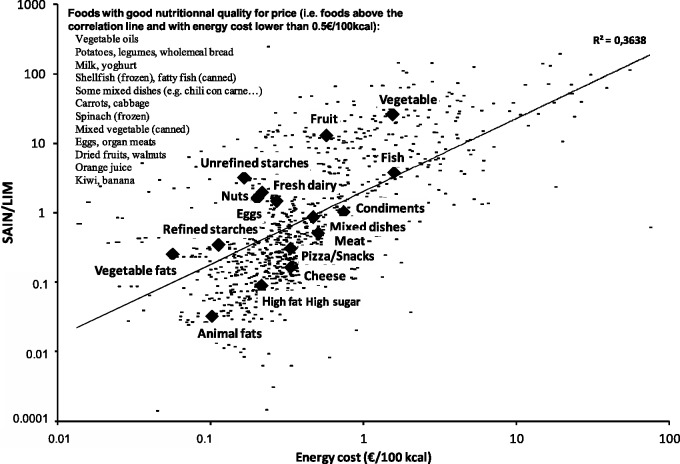
In order to have a balanced diet on a small budget, it is necessary to select particular foods with a very good ratio of nutritional quality to price. These foods have been identified by linear programming models42,112 or on the basis of favorable nutritional profiles.30,42,83 In general, pulses, nuts, oils, and whole-grain cereals were foods with very good ratios of nutritional quality to price. Among animal products, milk, eggs, poultry, organ meats, and canned sardines are also cited as foods with a good ratio of nutritional quality to price.42,83
Figure 4 shows the relation between nutrient quality of foods (estimated by the SAIN:LIM ratio) and energy cost (in €/100 kcal). Although the relation was positive, there was a wide dispersion around the regression line. Whereas certain foods (such as sweets) had a mediocre nutrition-to-price ratio, other foods had very favorable nutrition affordability metrics. Milk and carrots in particular offered optimal low-cost nutrition. Those foods were preferentially selected by linear programming models to construct nutritionally adequate diets at the lowest possible cost.42
Figure 4.
Foods with a good quality-to-price ratio in the French food database (n = 1117). Abbreviations: SAIN/LIM, Score of Nutritional Adequacy of Individual foods / score of nutrients to be LIMited
Do healthier diets have to cost more?
Although healthier diets generally cost more per calorie than do less-healthy diets, it is possible to eat better for less?25 For any level of diet quality, there will be a range of diet costs. Similarly, food patterns characterized by the same per-calorie diet cost can vary in quality. In general, creating food patterns that are both healthy and affordable may involve some compromises on taste, cost, convenience, and cultural acceptance. The USDA TFP129 was criticized for monotony and unappealing menus.133,134
Studies on the economic impact of improved diets have reported mixed results. In early studies, lower-fat diets were associated with higher food expenditures.135 Lower-income families in the United Kingdom136 and Denmark137 found some dietary interventions more difficult to follow because of their higher cost. However, other studies based on self-reports and small convenience samples claimed that better diets led to unchanged138,139 or even lower food expenditures.140,141 Results for the Mediterranean-style diets were equally mixed. Studies conducted in Spain showed that people who spontaneously adopted a Mediterranean diet spent more on food.31,95 By contrast, women who were encouraged to adopt a Mediterranean style diet in Canada did not report spending more.139
Although healthy food patterns generally costs more than less-healthy ones, there will be some that do not. A healthy Mediterranean-style diet can include seafood, salads, and scampi and be expensive, or rice, lentils, and beans and be cheap.142 Linear programming models aimed at generating nutritionally adequate food patterns at the lowest possible cost generally impose nutrition standards as well as cost and consumption constraints.112,113,131 Whereas healthy food patterns can be created relatively easily, the progressive introduction of cost constraints causes the optimized food patterns to depart sharply from existing ones. In other words, the modeled lower-cost food patterns can be nutritionally adequate, but at the cost of departing from social norms.112
Role of food substitution in diet quality and diet cost
One key question is whether substitution between similar food products allows consumers to obtain diets of comparable nutritional quality but at lower cost. People who need to reduce diet costs while maintaining existing food patterns begin by making substitutions within and eventually between food groups. In economic terms, foods that replace each other given a change in conditions are known as substitute goods. Thus, an increase in the price of whole fruit may drive consumers in the direction of fruit juices, with no consequences for diet quality or nutritional status. Indeed, lower–socioeconomic status groups consume more fruit juices, whereas higher–socioeconomic status groups consume more fruit.39
Study results on substitution effects have been inconsistent. McAllister et al.25 found that substitution of certain foods by their equivalents of better nutritional quality led to increased diet costs and no improvement in diet quality. A UK study of 5 food items (canned tomatoes, orange juice, potatoes, sausages, and sliced bread)143 suggests that substituting national brands with cheaper private labels would reduce costs without impacting nutritional quality because the prices of brand products could be up to 4 times higher than the cheaper products with a similar nutritional content.143
A study of 220 food products in France144 examined items in 17 product categories, such as cold meats, cooked dishes (such as cassoulet, ravioli, couscous, lentils, and sausages), desserts (such as chocolate cream, vanilla ice cream), etc. A nutrient quality score was derived on the basis of the list of ingredients and the calorie, protein, and lipid contents. Nutrient quality was significantly higher for the national brands, which were also considerably more expensive (by a factor of 2.5). Additional studies in France conducted by the Observatoire de la Qualité de l'Alimentation used food labels and price data to examine differences in nutrient composition by sale price.145 They confirmed that there was no systematic association between sale price and the fat, salt, or sugar content of food products of a particular type (e.g., corn flakes). Such price variability within the same narrow food category may explain why weak agreement was found between diets cost estimated with standard prices and those estimated with actual purchase prices.78,92,93.
By contrast, the prices of recommended foods in Australia were reported to be substantially higher than those of less-healthy options most markedly (30% difference) for legumes, canned fruit, beef, canned fish and margarine.146 In Canada, margarines rich in saturated and trans-fatty acids cost less than the others,147,148 and breads with whole-grain claims are less likely to be low in price than breads without such claims.149
Whether discount food should be recommended to lower-income consumers is a problematic issue. On one hand, processed and frozen vegetables and fruit provide comparable nutrition at lowest cost.87,150 On the other hand, some processed foods within the same food group may prove to be of lower nutritional quality than fresh foods. For instance, fresh fruit tends to provide greater nutrient content relative to canned options.151 It is very difficult to provide a clear-cut final answer to this question. The subject has been examined twice by the French National Food Council, in 20021 52 and in 2010.153 Both times, the conclusion was that existing data do not allow differences in the nutritional value of foods to be deduced from their differences in prices.
The high variability of food prices, both between and within food groups and between similar food items, may explain why wide variations in diet quality were observed at any level of cost.33,106 Overall, the studies showed that, although it was more difficult to obtain good nutrition at a moderate cost, two conditions made it theoretically feasible. The first condition was to have the food budget exceed the strict minimum required for fulfilling the nutritional recommendations.112 The second condition was to select foods with the highest nutrient-to-price ratio.42 Those population subgroups whose higher-quality diets were not associated with higher diet costs33,106 may well have made those selections. For example, Hispanic adults in the United States had higher-quality but lower-cost diets as compared with non-Hispanic adults.35,106 This was likely due to higher consumption of foods with a good ratio of nutritional quality to price.42,83,154
Linking food prices and diet quality with socioeconomic status
The literature shows that more-expensive and higher-quality diets were consumed by higher–socioeconomic status groups with better health outcomes. In the United States, food-insecure households had lower estimated diet costs, expressed in dollars per day and in dollars per 2000 kcal, based on analyses of the 2001–2002 NHANES database.35 In Sweden, the cheapest and most unhealthy diets were consumed by those children whose parents were the least educated and had manual and low-skill occupations.100 By contrast, higher–socioeconomic status groups in the United States had higher diet quality and higher estimated energy-adjusted diet costs.35 In other studies also, higher socioeconomic status was uniformly related to higher household food expenditures and to higher estimated diet costs.15,67,96,155 A study on supermarket baskets in Phoenix, Arizona, showed that shoppers of low socioeconomic status purchase calories in an inexpensive form that is higher in fat and less nutrient dense.70 Cross-sectional positive associations between diet quality and cost were also found within different socioeconomic status strata.65,96
The Seattle Obesity Study found that the relation between socioeconomic status and diet quality was attenuated once diet costs were included in the model.107 Socioeconomic status measures included education and incomes, whereas measures of diet quality were based on the mean adequacy ratio. First, there were significant positive correlations between socioeconomic status and diet quality, socioeconomic status and diet cost, and diet quality and diet cost, adjusting for numerous demographic covariates. The inclusion of the diet cost variable in the regression model attenuated the correlation between socioeconomic status and diet quality, suggesting that the impact of socioeconomic status variables on diet quality may be mediated by diet cost. This study103 was the first to provide empirical confirmation of hypotheses1,5,39 and models22,23 by showing that the cost of food contributed to explaining social inequalities with regard to nutrition. However, given the cross-sectional nature of the data, it was not possible to establish a causal link between the three factors studied: socioeconomic status, diet quality, and energy-adjusted diet cost.
Dietary guidelines for the prevention of noncommunicable diseases have emphasized the consumption of nutrient-rich foods and the selection of high-quality diets.116 Although this dietary advice has been aimed at all strata of society, diet quality also depends on socioeconomic status. Lower–socioeconomic status groups have lower-quality diets39 as well as higher rates of obesity, type 2 diabetes, and cardiovascular disease.156–158 By contrast, higher–socioeconomic status groups have better diets and better health.20,159 One explanation for the observed social gradient in diets and health is provided by disparate food prices and diet costs.1,5,67 The literature on the observed links between socioeconomic status, diet quality, and diet cost suggests some potential consequences for weights and health.11
Very few studies have related diet cost to health indicators. Studies based on cohorts of university students have found a negative correlation between energy cost, body mass index, and waist measurement in Japan108 and a positive association between low energy cost and 5-year weight gain in Spain.95 Finally, in a Greek cohort, no correlation was observed between food cost (in euros per week) and the 5-year incidence of cardiovascular disease.99 Longitudinal data have been scarce. By some reports, the lack of money at the end of the month led to a drop in fruit and vegetable consumption.160 Elsewhere, a drop in income161 or a loss of job security162 was found to be associated with weight gain.
CONCLUSION
Whether food prices pose a barrier to the adoption of healthier diets by lower-income groups was the specific question posed in this literature review. Evidence from the literature was provided to support the following points. First, the global hierarchy of food prices is such that energy-dense foods composed of refined grains, added sugars, or fats are cheaper per calorie than are the recommended nutrient-dense foods.30 Findings from multiple countries were unanimous on this point.
Second, lower-quality diets, with a higher content of added sugars and fats, were generally less expensive on a per-calorie basis. Those findings, based on data from multiple countries, essentially confirmed the early observations made in the United Kingdom by James et al.1
Third, cheaper and more energy-dense diets, often devoid of vegetables and fruit, tended to be selected across different countries by lower-income groups.39 Hidden hunger in poverty, even in developed nations, may be one result, since the lower-cost diets can be deficient in some key nutrients.29 There may also be a link between low-cost calories and high obesity rates.5,11,23
Fourth, the modeling of food patterns can help identify foods and combinations of foods that are affordable, nutrient rich, and culturally acceptable. In general, price reductions aimed at promoting healthier foods enhanced the impact of nutrition education163 and were more effective than education alone.164 Nonetheless, nutrition education should remain an important component of dietary guidance, since less-healthy food choices have also been shaped by the lack of nutrition knowledge, local attitudes, or by cultural norms.49,51,55,115,165 Some rarely eaten though nutritious foods may not find acceptance, and it is important to ensure that price-based interventions do not run counter to social and cultural norms.113
The present literature review has multiple implications for public policy. Published studies support the hypothesis that food prices affect diet quality and should be counted among the key socioeconomic determinants of health. In particular, the economic framework proposed in 20045,38 provides an explanation for the observed impact of socioeconomic status variables on diet quality, body weight, and health. Among factors predictive of obesity and related noncommunicable disease may be higher dietary energy density, lower nutrient density, and lower energy-adjusted diet cost.11,39
The argument that healthier diets cost more is politically charged and has attracted a significant amount of opposition, particularly in the United States. The key objections were grounded in the core belief that all segments of American society have the same degree of free choice, including the poor. “Poor people can afford a healthy diet but choose not to”44,166 was an often-repeated statement, as was the notion that getting maximum calories per dollar had no impact on food-purchase decisions.45
Opinions have evolved, however, and there is now at least a tacit understanding that nutrient-dense foods cost more, such that changing dietary behaviors may also require some economic interventions.167,168 For example, the stated intent of pricing interventions56,167,169 and food assistance programs170,171 is to promote purchases of vegetables and fruit by lower–socioeconomic status groups.163,164,172 There is an implicit assumption that the higher cost of vegetables and fruit may be a potential barrier to the adoption of healthier diets.48,59 Conversely, imposing taxes on beverages and snacks, a reverse economic intervention,173 was intended to restrict access to excessively cheap added sugars and fats by the same lower–socioeconomic status groups.174–177 However, not all food-based decisions stem from free choice. In a society of abundance, in which equal access to healthy diets is taken for granted, it is difficult to imagine that dietary guidelines cannot be followed by all socioeconomic status groups. Indeed, some dietary guidelines may increase social inequalities, since they are principally aimed at people of means.178 Regressive fiscal measures, including taxation, may also increase social inequalities in diet quality173 and so contribute to the already-widening gap in socioeconomic status–driven inequalities in health.179–182 New market-driven strategies, both behavioral and economic,183 but also human rights–based approaches and policies to ensure decent wages,118,184 may be needed to make nutrient-rich foods and high-quality diets equally available to all. At the same time, more research is needed to understand how some low-income individuals obtain higher-quality diets at no additional cost.185
Acknowledgments
The authors thank Wesley Tang, MPH, for assistance with the systematic review process.
Funding and sponsorship. The work of N.D. was supported by the Centre for Expertise Collective of INSERM. A.D. was supported by a National Institutes of Health grant DK076608-07.
Declaration of interest. The authors have no relevant interests to declare.
REFERENCES
- 1.James WP, Nelson M, Ralph A, et al. Socioeconomic determinants of health. The contribution of nutrition to inequalities in health. BMJ. 1997;314:1545–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.John Boyd O. Food, Health and Income: Report on a Survey of Adequacy of Diet in Relation to Income. London: MacMillan; 1936:71. [Google Scholar]
- 3.Orwell G. The Road to Wigan Pier. London: Victor Gollancz Ltd; 1937:86. [Google Scholar]
- 4.Wang DD, Leung CW, Li Y, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174:1587–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. [DOI] [PubMed] [Google Scholar]
- 6.McCrory MA, Saltzman E, Rolls BJ, et al. A twin study of the effects of energy density and palatability on energy intake of individual foods. Physiol Behav. 2006;87:451–459. [DOI] [PubMed] [Google Scholar]
- 7.Lissner L, Levitsky DA, Strupp BJ, et al. Dietary fat and the regulation of energy intake in human subjects. Am J Clin Nutr. 1987;46:886–892. [DOI] [PubMed] [Google Scholar]
- 8.Rolls BJ, Bell EA. Intake of fat and carbohydrate: role of energy density. Eur J Clin Nutr. 1999;53(suppl 1):S166–S173. [DOI] [PubMed] [Google Scholar]
- 9.Drewnowski A. Energy density, palatability, and satiety: implications for weight control. Nutr Rev. 1998;56:347–353. [DOI] [PubMed] [Google Scholar]
- 10.Drewnowski A. Fat and sugar: an economic analysis. J Nutr. 2003;133:838S–840S. [DOI] [PubMed] [Google Scholar]
- 11.Drewnowski A. The real contribution of added sugars and fats to obesity. Epidemiol Rev. 2007;29:160–171. [DOI] [PubMed] [Google Scholar]
- 12.Ledikwe JH, Blanck HM, Kettel KL, et al. Dietary energy density is associated with energy intake and weight status in US adults. Am J Clin Nutr. 2006;83:1362–1368. [DOI] [PubMed] [Google Scholar]
- 13.Northstone K, Emmett PM. Dietary patterns of men in ALSPAC: associations with socio-demographic and lifestyle characteristics, nutrient intake and comparison with women's dietary patterns. Eur J Clin Nutr. 2010;64:978–986. [DOI] [PubMed] [Google Scholar]
- 14.Malon A, Deschamps V, Salanave B, et al. Compliance with French nutrition and health program recommendations is strongly associated with socioeconomic characteristics in the general adult population. J Am Diet Assoc. 2010;110:848–856. [DOI] [PubMed] [Google Scholar]
- 15.Estaquio C, Druesne-Pecollo N, Latino-Martel P, et al. Socioeconomic differences in fruit and vegetable consumption among middle-aged French adults: adherence to the 5 A Day recommendation. J Am Diet Assoc. 2008;108:2021–2030. [DOI] [PubMed] [Google Scholar]
- 16.Lallukka T, Laaksonen M, Rahkonen O, et al. Multiple socio-economic circumstances and healthy food habits. Eur J Clin Nutr. 2007;61:701–710. [DOI] [PubMed] [Google Scholar]
- 17.Mullie P, Clarys P, Hulens M, et al. Dietary patterns and socioeconomic position. Eur J Clin Nutr. 2010;64:231–238. [DOI] [PubMed] [Google Scholar]
- 18.Harrington J, Fitzgerald AP, Layte R, et al. Sociodemographic, health and lifestyle predictors of poor diets. Public Health Nutr. 2011;14:2166–2175. [DOI] [PubMed] [Google Scholar]
- 19.McNaughton SA, Ball K, Crawford D, et al. An index of diet and eating patterns is a valid measure of diet quality in an Australian population. J Nutr. 2008;138:86–93. [DOI] [PubMed] [Google Scholar]
- 20.Kant AK, Graubard BI. Secular trends in the association of socio-economic position with self-reported dietary attributes and biomarkers in the US population: National Health and Nutrition Examination Survey (NHANES) 1971–1975 to NHANES 1999–2002. Public Health Nutr. 2007;10:158–167. [DOI] [PubMed] [Google Scholar]
- 21.Raffensperger S, Kuczmarski MF, Hotchkiss L, et al. Effect of race and predictors of socioeconomic status on diet quality in the HANDLS study sample. J Natl Med Assoc. 2010;102:923–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Darmon N, Ferguson EL, Briend A. A cost constraint alone has adverse effects on food selection and nutrient density: an analysis of human diets by linear programming. J Nutr. 2002;132:3764–3771. [DOI] [PubMed] [Google Scholar]
- 23.Darmon N, Ferguson E, Briend A. Do economic constraints encourage the selection of energy dense diets? Appetite. 2003;41:315–322. [DOI] [PubMed] [Google Scholar]
- 24.Butler P. Britain in nutrition recession as food prices rise and incomes shrink. The Guardian. November 18, 2012. http://www.theguardian.com/society/2012/nov/18/breadline-britain-nutritional-recession-austerity. Accessed July 16, 2015. [Google Scholar]
- 25.McAllister M, Baghurst KI, Record S. Financial costs of healthful eating: a comparison of three different approaches. J Nutr Educ. 1994;26:131–139. [Google Scholar]
- 26.Cade J, Upmeier H, Calvert C, et al. Costs of a healthy diet: analysis from the UK Women's Cohort Study. Public Health Nutr. 1999;2:505–512. [DOI] [PubMed] [Google Scholar]
- 27.Darmon N, Briend A, Drewnowski A. Energy-dense diets are associated with lower diet costs: a community study of French adults. Publ Health Nutr. 2004;7:21–27. [DOI] [PubMed] [Google Scholar]
- 28.Drewnowski A, Darmon N, Briend A. Replacing fats and sweets with vegetables and fruit – a question of cost. Am J Pub Health. 2004;94:1555–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andrieu E, Darmon N, Drewnowski A. Low-cost diets: more energy, fewer nutrients. Eur J Clin Nutr. 2006;60:434–436. [DOI] [PubMed] [Google Scholar]
- 30.Maillot M, Darmon N, Darmon M, et al. Nutrient-dense food groups have high energy costs: an econometric approach to nutrient profiling. J Nutr. 2007;137:1815–1820. [DOI] [PubMed] [Google Scholar]
- 31.Schroder H, Marrugat J, Covas MI. High monetary costs of dietary patterns associated with lower body mass index: a population-based study. Int J Obes. 2006;30:1574–1579. [DOI] [PubMed] [Google Scholar]
- 32.Lopez CN, Martinez-Gonzalez MA, Alonso A, et al. Cost of compliance with daily recommended values of micronutrients among a cohort of Spanish university graduates: the SUN (Seguimiento Universidad de Navarra) Study. Public Health Nutr. 2009;12:2092–2096. [DOI] [PubMed] [Google Scholar]
- 33.Bernstein AM, Bloom DE, Rosner BA, et al. Relation of food cost to healthfulness of diet among US women. Am J Clin Nutr. 2010;92:1197–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Monsivais P, Aggarwal A, Drewnowski A. Following federal guidelines to increase nutrient consumption may lead to higher food costs for consumers. Health Aff. 2011;30:1471–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rehm CD, Monsivais P, Drewnowski A. The quality and monetary value of diets consumed by adults in the United States. Am J Clin Nutr. 2011;94:1333–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rao M, Afshin A, Singh G, et al. Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis. BMJ Open. 2013;3:e004277 doi:10.1136/bmjopen-2013-004277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morris MA, Hulme C, Clarke GP, et al. What is the cost of a healthy diet? Using diet data from the UK Women's Cohort Study. J Epidemiol Commun Health. 2014;68:1043–1049. [DOI] [PubMed] [Google Scholar]
- 38.Drewnowski A, Darmon N. Food choices and diet costs: an economic analysis. J Nutr. 2005;135:900–904. [DOI] [PubMed] [Google Scholar]
- 39.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87:1107–1117. [DOI] [PubMed] [Google Scholar]
- 40.Dubuisson C, Lioret S, Touvier M, et al. Trends in food and nutritional intakes of French adults from 1999 to 2007: results from the INCA surveys. Br J Nutr. 2010;103:1035–1048. [DOI] [PubMed] [Google Scholar]
- 41.Darmon N, Vieux F, Maillot M, et al. Nutrient profiles discriminate between foods according to their contribution to nutritionally adequate diets: a validation study using linear programming and the SAIN,LIM system. Am J Clin Nutr. 2009;89:1227–1236. [DOI] [PubMed] [Google Scholar]
- 42.Maillot M, Ferguson EL, Drewnowski A, et al. Nutrient profiling can help identify foods of good nutritional quality for their price: a validation study with linear programming. J Nutr. 2008;138:1107–1113. [DOI] [PubMed] [Google Scholar]
- 43.Engel E. Die Productions und Consumtionsverhaltnisse des Königreichs Sachsen. In: von Holtzendorff F, Brentano L. (eds): Zeitschrift des Statistischen Büreaus des Königlich-Sächsischen Ministeriums des Innerns. Leipzig: Dunder and Humblot:1857;8–9. [Google Scholar]
- 44.Frazao E. Less-energy-dense diets of low-income women in California are associated with higher energy-adjusted costs but not with higher daily diet costs. Am J Clin Nutr. 2009;90:701–703. [DOI] [PubMed] [Google Scholar]
- 45.Lipsky LM. Are energy-dense foods really cheaper? Reexamining the relation between food price and energy density. Am J Clin Nutr. 2009;90:1397–1401. [DOI] [PubMed] [Google Scholar]
- 46.Caillavet F, Lecogne C, Nichèle V. La consommation alimentaire: des inégalités persistantes mais qui se réduisent. Cinquante ans de consommation en France [in French]. Paris: Insee; 2009.
- 47.Glanz K, Basil M, Maibach E, et al. Why Americans eat what they do: taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc. 1998;98:1118–1126. [DOI] [PubMed] [Google Scholar]
- 48.Lennernas M, Fjellstrom C, Becker W, et al. Influences on food choice perceived to be important by nationally- representative samples of adults in the European Union. Eur J Clin Nutr. 1997;51:S8–S15. [PubMed] [Google Scholar]
- 49.Dachner N, Ricciuto L, Kirkpatrick SI, et al. Food purchasing and food insecurity among low-income families in Toronto. Can J Diet Pract Res. 2010;71:e50–e56. [DOI] [PubMed] [Google Scholar]
- 50.Dowler E. Budgeting for food on a low income in the UK: the case of lone-parent families. Food Policy. 1997;22:405–417. [Google Scholar]
- 51.Wiig K, Smith C. The art of grocery shopping on a food stamp budget: factors influencing the food choices of low-income women as they try to make ends meet. Public Health Nutr. 2009;12:1726–1734. [DOI] [PubMed] [Google Scholar]
- 52.McLaughlin C, Tarasuk V, Kreiger N. An examination of at-home food preparation activity among low-income, food-insecure women. J Am Diet Assoc. 2003;103:1506–1512. [DOI] [PubMed] [Google Scholar]
- 53.Hampson SE, Martin J, Jorgensen J, et al. A social marketing approach to improving the nutrition of low-income women and children: an initial focus group study. Public Health Nutr. 2009;12:1563–1568. [DOI] [PubMed] [Google Scholar]
- 54.Leibtag ES, Kaufman PR. Exploring food purchase behavior of low-income households. How do they economize? In: Current Issues in Economics of Food Markets. Washington DC: Economic Research Service; 2003. Agriculture Information Bulletin no.747–07. [Google Scholar]
- 55.Inglis V, Ball K, Crawford D. Does modifying the household food budget predict changes in the healthfulness of purchasing choices among low- and high-income women? Appetite. 2009;52:273–279. [DOI] [PubMed] [Google Scholar]
- 56.Waterlander WE, de Mul A, Schuit AJ, et al. Perceptions on the use of pricing strategies to stimulate healthy eating among residents of deprived neighbourhoods: a focus group study. Int J Behav Nutr Phys Act. 2010;7:44 doi:10.1186/1479-5868-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dammann KW, Smith C. Factors affecting low-income women's food choices and the perceived impact of dietary intake and socioeconomic status on their health and weight. J Nutr Educ Behav. 2009;41:242–253. [DOI] [PubMed] [Google Scholar]
- 58.Durand-Gasselin S, Luquet FM. La vie quotidienne autour de l'alimentation. Les modes de vie, les représentations socio-culturelles et les comportements alimentaires de 55 familles à faibles revenus en banlieue parisienne. Med Nutr. 2000;1:40–52. [Google Scholar]
- 59.Beydoun MA, Wang Y. How do socio-economic status, perceived economic barriers and nutritional benefits affect quality of dietary intake among US adults? Eur J Clin Nutr. 2008; 62:303–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bowman SA. A comparison of the socioeconomic characteristics, dietary practices, and health status of women food shoppers with different food price attitudes. Nutr Res. 2006;26:318–324. [Google Scholar]
- 61.Aggarwal A, Monsivais P, Cook AJ, et al. Positive attitude toward healthy eating predicts higher diet quality at all cost levels of supermarkets. J Acad Nutr Diet. 2014;114:266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang KS. Nutrient elasticities in a complete food demand system. Am J Agric Econ. 1996;78:21–29. [Google Scholar]
- 63.Bowman SA. A methodology to price food consumed: development of a food price database. Fam Econ Nutr Rev. 1997;10:26–33. [Google Scholar]
- 64.Maillot M, Darmon N, Vieux F, et al. Low energy density and high nutritional quality are each associated with higher diet costs in French adults. Am J Clin Nutr. 2007;86:690–696. [DOI] [PubMed] [Google Scholar]
- 65.Townsend MS, Aaron GJ, Monsivais P, et al. Less-energy-dense diets of low-income women in California are associated with higher energy-adjusted diet costs. Am J Clin Nutr. 2009;89:1220–1226. [DOI] [PubMed] [Google Scholar]
- 66.Waterlander WE, de Haas WE, van Amstel I, et al. Energy density, energy costs and income – how are they related? Public Health Nutr. 2010;13:1599–1608. [DOI] [PubMed] [Google Scholar]
- 67.Aggarwal A, Monsivais P, Drewnowski A. Nutrient intakes linked to better health outcomes are associated with higher diet costs in the US. PLoS One. 2012;7:e37533 doi:10.1371/journal.pone.0037533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carlson A, Lino M, Juan W, et al. Development of the CNPP Prices Database. Washington, DC: US Department of Agriculture; 2008. [Google Scholar]
- 69.Darmon N, Darmon M, Maillot M, et al. A nutrient density standard for vegetables and fruits: nutrients per calorie and nutrients per unit cost. J Am Diet Assoc. 2005;105:1881–1887. [DOI] [PubMed] [Google Scholar]
- 70.Appelhans BM, Milliron BJ, Woolf K, et al. Socioeconomic status, energy cost, and nutrient content of supermarket food purchases. Am J Prev Med. 2012;42:398–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lakdawalla D, Philipson T. The growth of obesity and technological change. Econ Hum Biol. 2009;7:283–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chou S-Y, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Nutr. 2004;23:565–587. [DOI] [PubMed] [Google Scholar]
- 73.Monsivais P, Drewnowski A. The rising cost of low-energy-density foods. J Am Diet Assoc. 2007;107:2071–2076. [DOI] [PubMed] [Google Scholar]
- 74.Duffey KJ, Gordon-Larsen P, Shikany JM, et al. Food price and diet and health outcomes: 20 years of the CARDIA Study. Arch Intern Med. 2010;170:420–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.White House Task Force on Childhood Obesity. Solving the Problem of Childhood Obesity within a Generation. Report to the President. http://www.letsmove.gov/sites/letsmove.gov/files/TaskForce_on_Childhood_Obesity_May2010_FullReport.pdf. Published 2010. Accessed July 16, 2015. [DOI] [PubMed]
- 76.Jones NR, Conklin AI, Suhrcke M, et al. The growing price gap between more and less healthy foods: analysis of a novel longitudinal UK dataset. PLoS One. 2014;9:e109343 doi:10.1371/journal.pone.0109343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Combris P. Le poids des contraintes économiques dans les choix alimentaires. [Impact of economic constraints on food choices]. Cah Nutr Diet. 2012;2006:279–284. [Google Scholar]
- 78.Timmins KA, Morris MA, Hulme C, et al. Comparability of methods assigning monetary costs to diets: derivation from household till receipts versus cost database estimation using 4-day food diaries. Eur J Clin Nutr. 2013;67:1072–1076. [DOI] [PubMed] [Google Scholar]
- 79.Drewnowski A. The cost of US foods as related to their nutritive value. Am J Clin Nutr. 2010;92:1181–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Darmon N, Maillot M. In foods, energy is cheap where it is abundant and expensive where it is scarce: this is a fact, not an artifact. Am J Clin Nutr. 2010;91:1068–1069. [DOI] [PubMed] [Google Scholar]
- 81.Brimblecombe JK, O'Dea K. The role of energy cost in food choices for an Aboriginal population in northern Australia. Med J Aust. 2009;190:549–551. [DOI] [PubMed] [Google Scholar]
- 82.Drewnowski A, Maillot M, Darmon N. Testing nutrient profile models in relation to energy density and energy cost. Eur J Clin Nutr. 2009;63:674–683. [DOI] [PubMed] [Google Scholar]
- 83.Drewnowski A. The Nutrient Rich Foods Index helps to identify healthy, affordable foods. Am J Clin Nutr. 2010;91:1095S–1101S. [DOI] [PubMed] [Google Scholar]
- 84.Drewnowski A, Fulgoni V., III Nutrient profiling of foods: creating a nutrient-rich foot index. Nutr Rev. 2008;66:23–39. [DOI] [PubMed] [Google Scholar]
- 85.Fulgoni VL, III, Keast DR, Drewnowski A. Development and validation of the nutrient-rich foods index: a tool to measure nutritional quality of foods. J Nutr. 2009;139:1549–1554. [DOI] [PubMed] [Google Scholar]
- 86.Darmon N. We eat foods, we need nutrients (comment on “The good, the bad, and the ultra-processed” by Carlos Monteiro). Public Health Nutr. 2009;12:1967–1968. [DOI] [PubMed] [Google Scholar]
- 87.Drewnowski A. New metrics of affordable nutrition: which vegetables provide most nutrients for least cost? J Acad Nutr Diet. 2013;113:1182–1187. [DOI] [PubMed] [Google Scholar]
- 88.Lee A, Mhurchu CN, Sacks G, et al. Monitoring the price and affordability of foods and diets globally. Obes Rev. 2013;14(suppl 1):82–95. [DOI] [PubMed] [Google Scholar]
- 89.Neuhouser ML, Kristal AR, McLerran D, et al. Validity of short food frequency questionnaires used in cancer chemoprevention trials: results from the Prostate Cancer Prevention Trial. Cancer Epidemiol Biomarkers Prev. 1999;8:721–725. [PubMed] [Google Scholar]
- 90.Ambrosini GL, Mackerras D, de Klerk NH, et al. Comparison of an Australian food-frequency questionnaire with diet records: implications for nutrition surveillance. Public Health Nutr. 2003;6:415–422. [DOI] [PubMed] [Google Scholar]
- 91.Erkkola M, Karppinen M, Javanainen J, et al. Validity and reproducibility of a food frequency questionnaire for pregnant Finnish women. Am J Epidemiol. 2001;154:466–476. [DOI] [PubMed] [Google Scholar]
- 92.Monsivais P, Perrigue MM, Adams SL, et al. Measuring diet cost at the individual level: a comparison of three methods. Eur J Clin Nutr. 2013;67:1220–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Aaron GJ, Keim NL, Drewnowski A, et al. Estimating dietary costs of low-income women in California: a comparison of 2 approaches. Am J Clin Nutr. 2013;97:835–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.US Department of Agriculture, Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies, 1.0 – Documentation and User Guide. Beltsville, MD: Agricultural Research Service, Food Surveys Research Group; 2004. [Google Scholar]
- 95.Lopez CN, Martinez-Gonzalez MA, Sanchez-Villegas A, et al. Costs of Mediterranean and Western dietary patterns in a Spanish cohort and their relationship with prospective weight change. J Epidemiol Commun Health. 2009;63:920–927. [DOI] [PubMed] [Google Scholar]
- 96.Monsivais P, Drewnowski A. Lower-energy-density diets are associated with higher monetary costs per kilocalorie and are consumed by women of higher socioeconomic status. J Am Diet Assoc. 2009;109:814–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Murakami K, Sasaki S, Takahashi Y, et al. Monetary cost of self-reported diet in relation to biomarker-based estimates of nutrient intake in young Japanese women. Public Health Nutr. 2009;12:1290–1297. [DOI] [PubMed] [Google Scholar]
- 98.Murakami K, Sasaki S, Takahashi Y, et al. Monetary cost of dietary energy is negatively associated with BMI and waist circumference, but not with other metabolic risk factors, in young Japanese women. Public Health Nutr. 2009;12:1092–1098. [DOI] [PubMed] [Google Scholar]
- 99.Vlismas K, Panagiotakos DB, Pitsavos C, et al. Quality, but not cost, of diet is associated with 5-year incidence of CVD: the ATTICA study. Public Health Nutr. 2010;13:1890–1897. [DOI] [PubMed] [Google Scholar]
- 100.Ryden PJ, Hagfors L. Diet cost, diet quality and socio-economic position: how are they related and what contributes to differences in diet costs? Public Health Nutr. 2011;14:1680–1692. [DOI] [PubMed] [Google Scholar]
- 101.Margetts BM, Nelson M. Design Concepts in Nutritional Epidemiology. 2nd ed Oxford: Oxford University Press; 1997:468. [Google Scholar]
- 102.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124:17–27. [DOI] [PubMed] [Google Scholar]
- 103.Aggarwal A, Monsivais P, Cook AJ, et al. Does diet cost mediate the relation between socioeconomic position and diet quality? Eur J Clin Nutr. 2011;65:1059–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cade J, Booth S. What can people eat to meet the dietary goals: and how much does it cost? J Hum Nutr Diet. 1990;3:199–207. [Google Scholar]
- 105.Schroder H, Vila J, Marrugat J, et al. Low energy density diets are associated with favorable nutrient intake profile and adequacy in free-living elderly men and women. J Nutr. 2008;138:1476–1481. [DOI] [PubMed] [Google Scholar]
- 106.Monsivais P, Rehm CD, Drewnowski A. The DASH diet and diet costs among ethnic and racial groups in the United States. JAMA Intern Med. 2013;173:1922–1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Monsivais P, Aggarwal A, Drewnowski A. Are socio-economic disparities in diet quality explained by diet cost? [published online ahead of print December 10, 2010]. J Epidemiol Community Health. 2012;66:530–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Murakami K, Sasaki S, Okubo H, et al. Monetary costs of dietary energy reported by young Japanese women: association with food and nutrient intake and body mass index. Public Health Nutr. 2007;10:1430–1439. [DOI] [PubMed] [Google Scholar]
- 109.Keim NL, Forester SM, Lyly M, et al. Vegetable variety is a key to improved diet quality in low-income women in California. J Acad Nutr Diet. 2014;114:430–435. [DOI] [PubMed] [Google Scholar]
- 110.Stigler GJ. The cost of subsistence. J Farm Econ. 1945;27:303–314. [Google Scholar]
- 111.Dantzig GB. The diet problem. Interfaces. 2002;20:43–47. [Google Scholar]
- 112.Darmon N, Ferguson EL, Briend A. Impact of a cost constraint on nutritionally adequate food choices for French women: an analysis by linear programming. J Nutr Educ Behav. 2006;38:82–90. [DOI] [PubMed] [Google Scholar]
- 113.Maillot M, Darmon N, Drewnowski A. Are the lowest-cost healthful food plans culturally and socially acceptable? Public Health Nutr. 2010;13:1178–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lino M. The Thrifty Food Plan, 1999: revisions of the market baskets. Fam Econ Nutr Rev. 2001;13:50–63. [Google Scholar]
- 115.Dowler E, Barlösius E, Feichtinger E, et al. Poverty, food and nutrition. In: Köhler BM, Feichtinger E, Barlösius E, et al., eds. Poverty and Food in Welfare Societies. Berlin: Sigma;1997:17–30. [Google Scholar]
- 116.World Health Organization. Global Strategy on Diet, Physical Activity and Health. Geneva: World Health Organization; 2004. [Google Scholar]
- 117.Rolls BJ, Drewnowski A, Ledikwe JH. Changing the energy density of the diet as a strategy for weight management. J Am Diet Assoc. 2005;105(suppl):S98–S103. [DOI] [PubMed] [Google Scholar]
- 118.Morris JN, Donkin AJ, Wonderling D, et al. A minimum income for healthy living. J Epidemiol Commun Health. 2000;54:885–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Morris J, Wilkinson P, Dangour AD, et al. Defining a minimum income for healthy living (MIHL): older age, England. Int J Epidemiol. 2007;36:1300–1307. [DOI] [PubMed] [Google Scholar]
- 120.Nelson M, Dick K, Holmes B. Food budget standards and dietary adequacy in low-income families. Proc Nutr Soc. 2002;61:569–577. [DOI] [PubMed] [Google Scholar]
- 121.Vozoris N, Davis B, Tarasuk V. The affordability of a nutritious diet for households on welfare in Toronto. Can J Public Health. 2002;93:36–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Williams PL, Johnson CP, Kratzmann ML, et al. Can households earning minimum wage in Nova Scotia afford a nutritious diet? Can J Public Health. 2006;97:430–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Friel S, Walsh O, McCarthy D. The irony of a rich country: issues of financial access to and availability of healthy food in the Republic of Ireland. J Epidemiol Commun Health. 2006;60:1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kettings C, Sinclair AJ, Voevodin M. A healthy diet consistent with Australian health recommendations is too expensive for welfare-dependent families. Aust N Z J Public Health. 2009;33:566–572. [DOI] [PubMed] [Google Scholar]
- 125.Rose D, Charlton KE. Quantitative indicators from a food expenditure survey can be used to target the food insecure in South Africa. J Nutr. 2002;132:3235–3242. [DOI] [PubMed] [Google Scholar]
- 126.Cassady D, Jetter KM, Culp J. Is price a barrier to eating more fruits and vegetables for low-income families? J Am Diet Assoc. 2007;107:1909–1915. [DOI] [PubMed] [Google Scholar]
- 127.Martin A. Nutritional recommendations for the French population. Sciences des Aliments. 2001;21:317–458. [Google Scholar]
- 128.Castetbon K, Mejean C, Deschamps V, et al. Dietary behaviour and nutritional status in underprivileged people using food aid (ABENA study, 2004–2005). J Hum Nutr Diet. 2011;24:560–571. [DOI] [PubMed] [Google Scholar]
- 129.US Department of Agriculture. USDA food plans: cost of food. http://www.cnpp.usda.gov/USDAFoodPlansCostofFood. Accessed July 16, 2015. [Google Scholar]
- 130.US Department of Agriculture, Economic Research Service. Per capita food expenditures in the US. ERS Food Expenditure Series, Table 13. http://www.ers.usda.gov/data-products/food-expenditures.aspx#.UwlLSPldVMU. Published December 1, 2014. Accessed July 16, 2015. [Google Scholar]
- 131.Wilde PE, Llobrera J. Using the Thrifty Food Plan to assess the cost of a nutritious diet. J Consum Aff. 2009;43:274–304. [Google Scholar]
- 132.Neault N, Cook JT, Morris V, et al. The real cost of a healthy diet: healthful foods are out of reach for low income families in Boston, Massachusetts. http://dcc2 bumc bu edu/csnappublic/HealthyDiet_Aug2005 pdf 2005; Report published August 2005 by the Boston Medical Center Department of Pediatrics. [Google Scholar]
- 133.You W, Zhang G, Davy BM, et al. Food consumed away from home can be a part of a healthy and affordable diet. J Nutr. 2009;139:1994–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Davis GC, You W. The Thrifty Food Plan is not thrifty when labor cost is considered. J Nutr. 2010;140:854–857. [DOI] [PubMed] [Google Scholar]
- 135.Lloyd HM, Paisley CM, Mela DJ. Barriers to the adoption of reduced-fat diets in a UK population. J Am Diet Assoc. 1995;95:316–322. [DOI] [PubMed] [Google Scholar]
- 136.MacDonald A, Forsythe WI. The cost of nutrition and diet therapy for low-income families. Hum Nutr Appl Nutr. 1986;40:87–96. [PubMed] [Google Scholar]
- 137.Stender S, Skovby F, Haraldsdottir J, et al. Cholesterol-lowering diets may increase the food costs for Danish children. A cross-sectional study of food costs for Danish children with and without familial hypercholesterolaemia. Eur J Clin Nutr. 1993;47:776–786. [PubMed] [Google Scholar]
- 138.Mitchell DC, Shannon BM, McKenzie J, et al. Lower fat diets for children did not increase food costs. J Nutr Educ Behav. 2000;32:100–103. [Google Scholar]
- 139.Goulet J, Lamarche B, Lemieux S. A nutritional intervention promoting a Mediterranean food pattern does not affect total daily dietary cost in North American women in free-living conditions. J Nutr. 2008;138:54–59. [DOI] [PubMed] [Google Scholar]
- 140.Burney J, Haughton B. EFNEP: a nutrition education program that demonstrates cost-benefit. J Am Diet Assoc. 2002;102:39–45. [DOI] [PubMed] [Google Scholar]
- 141.Ottelin AM, Lindstrom J, Peltonen M, et al. Costs of a self-selected, health-promoting diet among the participants of the Finnish Diabetes Prevention Study. Diabetes Care. 2007;30:1275–1277. [DOI] [PubMed] [Google Scholar]
- 142.Drewnowski A, Eichelsdoerfer P. The Mediterranean diet: does it have to cost more? Public Health Nutr. 2009;12:1621–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cooper S, Nelson M. ‘Economy' line foods from four supermarkets and brand name equivalents: a comparison of their nutrient contents and costs. J Hum Nutr Diet. 2003;16:339–347. [DOI] [PubMed] [Google Scholar]
- 144.Darmon N, Caillavet F, Joly C, et al. Low-cost foods: how do they compare with their brand name equivalents? A French study. Public Health Nutr 2009;12:808–815. [DOI] [PubMed] [Google Scholar]
- 145.Menard C, Dumas C, Gillot N, et al. The French OQALI survey on dairy products: comparison of nutrient contents and other nutrition information on labels among types of brands. J Hum Nutr Diet. 2012;25:323–333. [DOI] [PubMed] [Google Scholar]
- 146.Giskes K, Van Lenthe FJ, Brug J, et al. Socioeconomic inequalities in food purchasing: the contribution of respondent-perceived and actual (objectively measured) price and availability of foods. Prev Med. 2007;45:41–48. [DOI] [PubMed] [Google Scholar]
- 147.Ricciuto L, Ip H, Tarasuk V. The relationship between price, amounts of saturated and trans fats, and nutrient content claims on margarines and oils. Can J Diet Pract Res. 2005;66:252–255. [DOI] [PubMed] [Google Scholar]
- 148.Ricciuto L, Lin K, Tarasuk V. A comparison of the fat composition and prices of margarines between 2002 and 2006, when new Canadian labelling regulations came into effect. Public Health Nutr. 2009;12:1270–1275. [DOI] [PubMed] [Google Scholar]
- 149.Sumanac D, Mendelson R, Tarasuk V. Marketing whole grain breads in Canada via food labels. Appetite. 2013;62:1–6. [DOI] [PubMed] [Google Scholar]
- 150.Drewnowski A, Rehm CD. Vegetable cost metrics show that potatoes and beans provide most nutrients per penny. PLoS One. 2013;8:e63277 doi:10.1371/journal.pone.0063277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Miller SR, Knudson WA. Nutrition and cost comparisons of select canned, frozen, and fresh fruits and vegetables. Am J Lifestyle Med. 2014;8:430–437. [Google Scholar]
- 152.Groupe de travail réuni par le CNA. Avis sur l'exclusion sociale et l'alimentation. Paris: Conseil National de l'Alimentation (CNA); 2002. Avis no. 34:2002. [Google Scholar]
- 153.Groupe de travail réuni par le CNA. Qualité nutritionnelle, consommation et distribution des produits alimentaires “hard discount” et “premiers prix": état des lieux et perspectives. Paris: Conseil National de l'Alimentation (CNA); 2010. Avis no. 67:2010. [Google Scholar]
- 154.Mitchell DC, Lawrence FR, Hartman TJ, et al. Consumption of dry beans, peas, and lentils could improve diet quality in the US population. J Am Diet Assoc. 2009;109:909–913. [DOI] [PubMed] [Google Scholar]
- 155.Timmins KA, Hulme C, Cade JE. The monetary value of diets consumed by British adults: an exploration into sociodemographic differences in individual-level diet costs [published online ahead of print October 29, 2013]. Public Health Nutr. 2015;18:151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Brown AF, Ettner SL, Piette J, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004;26:63–77. [DOI] [PubMed] [Google Scholar]
- 157.Charles MA, Eschwege E, Basdevant A. Monitoring the obesity epidemic in France: the Obepi surveys 1997–2006. Obesity. 2008;16:2182–2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Marmot M, Allen J, Bell R, et al. WHO European review of social determinants of health and the health divide. Lancet. 2012;380:1011–1029. [DOI] [PubMed] [Google Scholar]
- 159.Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358:2468–2481. [DOI] [PubMed] [Google Scholar]
- 160.Tarasuk V, McIntyre L, Li J. Low-income women's dietary intakes are sensitive to the depletion of household resources in one month. J Nutr. 2007;137:1980–1987. [DOI] [PubMed] [Google Scholar]
- 161.Köhler BM, Feichtinger E, Barlösius E, et al., eds. Poverty and Food in Welfare Societies. Berlin: Sigma; 1997. [Google Scholar]
- 162.Ferrie JE, Shipley MJ, Marmot MG, et al. An uncertain future: the health effects of threats to employment security in white-collar men and women. Am J Public Health. 1998;88:1030–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Anderson JV, Bybee DI, Brown RM, et al. 5 a day fruit and vegetable intervention improves consumption in a low income population. J Am Diet Assoc. 2001;101:195–202. [DOI] [PubMed] [Google Scholar]
- 164.Burr ML, Trembeth J, Jones KB, et al. The effects of dietary advice and vouchers on the intake of fruit and fruit juice by pregnant women in a deprived area: a controlled trial. Public Health Nutr 2007;10:559–565. [DOI] [PubMed] [Google Scholar]
- 165.Le J, Dallongeville J, Wagner A, et al. Attitudes toward healthy eating: a mediator of the educational level–diet relationship. Eur J Clin Nutr. 2013;67:808–814. [DOI] [PubMed] [Google Scholar]
- 166.Reed J, Frazão E, Istkowitz R. How Much Do Americans Pay for Fruits and Vegetables? Washington, DC: US Department of Agriculture, Economic Research Service; 2004. Agriculture Information Bulletin no. 790. [Google Scholar]
- 167.Epstein LH, Jankowiak N, Nederkoorn C, et al. Experimental research on the relation between food price changes and food-purchasing patterns: a targeted review [published online ahead of print February 29, 2012]. Am J Clin Nutr. 2015;95:789–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Waterlander WE, Steenhuis IH, de Boer MR, et al. The effects of a 25% discount on fruits and vegetables: results of a randomized trial in a three-dimensional web-based supermarket. Int J Behav Nutr Phys Act. 2012;9:11 doi:10.1186/1479-5868-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Waterlander WE, de Boer MR, Schuit AJ, et al. Price discounts significantly enhance fruit and vegetable purchases when combined with nutrition education: a randomized controlled supermarket trial. Am J Clin Nutr. 2013;97:886–895. [DOI] [PubMed] [Google Scholar]
- 170.Herman DR, Harrison GG, Afifi AA, et al. Effect of a targeted subsidy on intake of fruits and vegetables among low-income women in the Special Supplemental Nutrition Program for Women, Infants, and Children. Am J Public Health. 2008;98:98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Han E, Powell LM, Isgor Z. Supplemental nutrition assistance program and body weight outcomes: the role of economic contextual factors. Soc Sci Med. 2012;74:1874–1881. [DOI] [PubMed] [Google Scholar]
- 172.Herman DR, Harrison GG, Jenks E. Choices made by low-income women provided with an economic supplement for fresh fruit and vegetable purchase. J Am Diet Assoc. 2006;106:740–744. [DOI] [PubMed] [Google Scholar]
- 173.Darmon N, Lacroix A, Muller L, et al. Food price policies improve diet quality while increasing socioeconomic inequalities in nutrition. Int J Behav Nutr Phys Act. 2014;11:66 doi:10.1186/1479-5868-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wall J, Mhurchu CN, Blakely T, et al. Effectiveness of monetary incentives in modifying dietary behavior: a review of randomized, controlled trials. Nutr Rev. 2006;64:518–531. [DOI] [PubMed] [Google Scholar]
- 175.Andreyeva T, Chaloupka FJ, Brownell KD. Estimating the potential of taxes on sugar-sweetened beverages to reduce consumption and generate revenue. Prev Med. 2011;52:413–416. [DOI] [PubMed] [Google Scholar]
- 176.Mytton O, Gray A, Rayner M, et al. Could targeted food taxes improve health? J Epidemiol Community Health. 2007;61:689–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98:216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mackenbach JP, Bos V, Andersen O, et al. Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol. 2003;32:830–837. [DOI] [PubMed] [Google Scholar]
- 180.LeClerc A, Chastang JF, Menvielle G, et al. Socioeconomic inequalities in premature mortality in France: have they widened in recent decades? Soc Sci Med. 2006; 62:2035–2045. [DOI] [PubMed] [Google Scholar]
- 181.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol. 2010;20:40–52. [DOI] [PubMed] [Google Scholar]
- 182.Singh GK, Siahpush M. Widening socioeconomic inequalities in US life expectancy, 1980–2000. Int J Epidemiol. 2006;35:969–979. [DOI] [PubMed] [Google Scholar]
- 183.Brambila-Macias J, Shankar B, Capacci S, et al. Policy interventions to promote healthy eating: a review of what works, what does not, and what is promising. Food Nutr Bull. 2011;32:365–375. [DOI] [PubMed] [Google Scholar]
- 184.Dowler EA, O'Connor D. Rights-based approaches to addressing food poverty and food insecurity in Ireland and UK. Soc Sci Med. 2012;74:44–51. [DOI] [PubMed] [Google Scholar]
- 185.Marty L, Dubois C, Gaubard MS, et al. Higher nutritional quality at no additional cost among low-income households: insights from food purchases of “positive deviants.” Am J Clin Nutr 2015;102:190–198. [DOI] [PubMed] [Google Scholar]