Abstract
This population-based study examines the availability of broadband in local communities for telemedicine.
Access to health specialists is difficult for many individuals in rural communities.1 Telemedicine, health care service delivered remotely through telecommunications, is one potential solution, but its use varies across regions, potentially associated with the availability of high-speed internet (broadband) access.2 The Federal Communications Commission (FCC) and Congress have emphasized the need to increase broadband access in rural communities, in part to facilitate the use of telemedicine, and the FCC’s Connect America Fund has set aside billions of dollars to subsidize broadband expansion.3 Our objective was to examine whether broadband availability in local communities is associated with telemedicine use.
Methods
This study was approved by the Harvard Medical School Institutional Review Board, which waived the requirement for informed patient consent because of deidentified data. Per capita rates of telemedicine visits for each US county in 2016 were calculated using a nationally representative 20% sample of Medicare fee-for-service beneficiaries and data from OptumLabs Data Warehouse, a deidentified claims database for privately insured enrollees and Medicare Advantage enrollees in a large, private US health plan. Telemedicine visits were defined as health professional claims with either a telemedicine modifier (GT, GQ, 95) or a telemedicine-specific code (G0425-7, G0406-8, or G0459). Counts of visits were based on the beneficiary’s county of residence. Because Medicare does not cover telemedicine for nonrural beneficiaries living in metropolitan counties, we did not include these beneficiaries in our per capita rates. We removed counties without rural residents, without both commercial and Medicare beneficiaries, and outlier counties in the top percentile of per capita telemedicine use.
We measured broadband availability at the county level using the FCC’s Fixed Broadband Deployment Data.4 Broadband access was defined as the availability of wired internet download speeds of at least 25 megabytes per second and upload speeds of at least 3 megabytes per second.5 Counties were categorized based on the share of the county’s population that could purchase broadband: low availability (0%-40%), medium availability (>40%-70%), or high availability (>70%). In each county, we also determined the number of census blocks targeted by the FCC’s Connect America Fund.
We split our sample of counties (N = 2785) into 3 groups based on their level of rurality using 2013 Department of Agriculture’s Rural-Urban Continuum Codes,6 including metropolitan counties with rural residents (codes 1-3), nonmetropolitan counties (4-7) with smaller towns/cities (≥2500 urban residents), and nonmetropolitan counties (8-9) without urban areas (ie, fully rural). In each subsample of counties, we predicted per 1000 beneficiary telemedicine rates at each broadband category using negative binomial regressions, controlling for county level socioeconomic characteristics, per capita hospitals, health centers and psychiatrists, and state level differences in commercial reimbursement regulations for telemedicine (Table). Sensitivity analyses examined the Medicare and commercial population separately. P values <.05 were considered significant. Analysis was conducted using Stata, version 14 (StataCorp LLC).
Table. Characteristics of Counties Stratified by Level of Ruralitya.
| Variable | Metropolitan Counties With Rural Residentsb | Nonmetropolitan Countiesb | |
|---|---|---|---|
| With Smaller Towns/Cities | Fully Rural | ||
| Counties, No. | 869 | 1317 | 599 |
| Broadband availability, No. (%) of countiesc | |||
| Low (0%-40%) | 86 (9.9) | 236 (17.9) | 297 (49.6) |
| Medium (>40%-70%) | 146 (16.8) | 465 (35.3) | 143 (23.9) |
| High (>70%) | 637 (73.3) | 616 (46.8) | 159 (26.5) |
| Telemedicine visits per 1000 beneficiaries, No., mean (SD)d | 4.2 (6.4) | 13.1 (17.0) | 16.9 (23.3) |
| Medicare | 29.1 (102.0) | 25.1 (37.1) | 27.6 (43.3) |
| Commercial | 3.0 (4.2) | 6.4 (11.3) | 10.0 (22.3) |
| County characteristics, No., mean (SD) | |||
| Population, mean | 197 211 (487 573) | 31 372 (22 661) | 7674 (5790) |
| Fraction of county rural, No. (%) | 43.3 (30.3) | 56.2 (18.5) | 99.3 (4.2) |
| Population density, per km2 | 100.5 (160.4) | 20.4 (27.5) | 6.1 (6.7) |
| Age, y, No. (%) | |||
| <18 | 23.1 (3.0) | 22.7 (3.2) | 21.8 (3.9) |
| 18-64 | 61.4 (3.2) | 59.9 (3.3) | 57.4 (3.8) |
| ≥65 | 15.4 (3.7) | 17.3 (3.6) | 20.6 (4.6) |
| Male, No. (%) | 49.5 (1.8) | 50.2 (2.5) | 50.5 (2.9) |
| White race, No. (%) | 82.2 (14.4) | 84.5 (16.1) | 87.4 (17.2) |
| Hispanic ethnicity, No. (%) | 9.4 (13.1) | 9.4 (15.1) | 6.1 (11.1) |
| High school graduate, No. (%) | 86.6 (5.6) | 84.0 (6.9) | 85.1 (7.1) |
| Income to poverty ratio, No. (%) | |||
| <100 | 15.6 (5.4) | 18.1 (6.4) | 17.0 (7.6) |
| 100-149 | 9.9 (2.6) | 11.7 (2.9) | 12.0 (3.6) |
| ≥150 | 74.3 (7.4) | 70.1 (8.3) | 70.9 (9.6) |
| Health centers (per 100 000) | 9.6 (14.3) | 16.4 (16.2) | 42.4 (48.2) |
| Hospitals (per 100 000) | 2.9 (5.3) | 8.7 (8.9) | 21.2 (30.6) |
| Psychiatrists (per 100 000) | 5.5 (7.7) | 2.5 (4.8) | 0.7 (3.3) |
| State mandate that health plans reimburse for video telemedicine visits, No. (%)e | |||
| No mandate | 526 (60.5) | 763 (57.9) | 311 (51.9) |
| Conditional mandate | 79 (9.1) | 124 (9.4) | 86 (14.4) |
| Mandate | 193 (22.2) | 299 (22.7) | 126 (21.0) |
| Parity | 71 (8.2) | 132 (10.0) | 76 (12.7) |
| FCC Connect America Fund Phase II auctionf | |||
| Supported population, No. | 427 800 | 634 312 | 124 342 |
| Total supported population, % | 36.1 | 53.5 | 10.5 |
| Annual supported amount, $ millions | 44.2 | 74.2 | 22.8 |
| % of total support | 31.3 | 52.6 | 16.1 |
County level characteristics were obtained from the 2016 Area Health Resources File and American Community Survey.6
County levels of rurality were obtained from the 2013 Rural-Urban Continuum Codes.
Fixed Broadband Deployment Data (current as of December 2015).4
Per capita telemedicine visit rates are from 2016.
State regulations on commercial reimbursement were obtained from the September 2014 state telehealth laws and Medicaid program policies report from the Center for Connected Health Policy. No mandate indicates the state had no regulation on commercial reimbursement for live video telemedicine; mandate, the state had a regulation compelling reimbursement; conditional mandate, there was a mandate but with conditions; and parity, commercial payers must pay for telemedicine visits at a rate equal to in-person visits.
County-level auction data on supported areas were obtained from block-level Connect America Fund data.3
Results
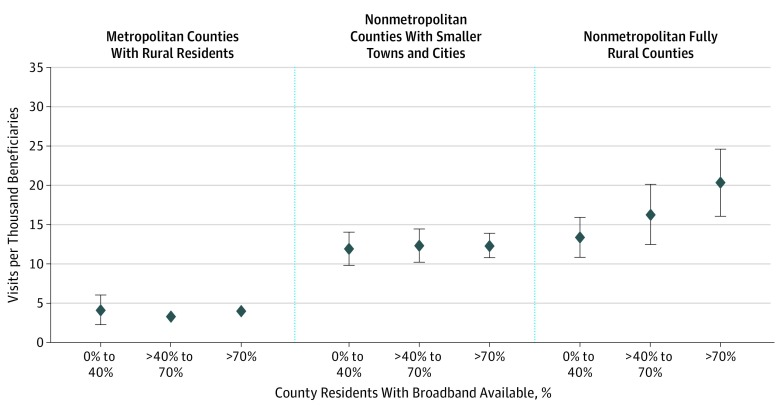
Our sample consisted of 869 metropolitan counties with at least some rural residents, 1317 nonmetropolitan counties with smaller towns/cities, and 599 fully rural counties.6 In fully rural counties, greater broadband access was associated with greater telemedicine use: counties with low broadband availability had 34% fewer visits per capita compared with counties with high broadband availability (13.4 per 1000 vs 20.4, P = .004) (Figure). In metropolitan counties with rural residents and nonmetropolitan counties with smaller towns/cities, greater broadband access was not associated with differences in telemedicine use. For example, in metropolitan counties with rural residents, counties with low vs high broadband availability had 2.4% more visits per capita (4.2 vs 4.1 per 1000; P > .99). Results were consistent when we modeled commercial and Medicare rates separately or used different cutoffs for broadband availability. Of the FCC’s Connect America Fund investment, 16.1% was to fully rural counties.
Figure. Predicted per Capita Telemedicine Visits in 2016 Stratified by Type of County and Broadband Availability, Adjusted for Other County Characteristics.
Regression analysis was conducted at the county level. Primary outcome was per capita telemedicine visits per 1000 Medicare and commercial beneficiaries combined. County broadband availability was aggregated up from census blocks by block population. Negative binomial regressions with robust SEs were adjusted for county population and density, percent rural, age group (<18, 18-64, ≥65), sex, white, Hispanic, high school educated, income to poverty group (<100%, 100%-149%, ≥150%), per capita number of health centers, hospitals and psychiatrists, and indicators for state laws on whether health plans must reimburse video telemedicine visits. Predictions were taken at sample means and are shown with diamonds. Bars surrounding each prediction are 95% CIs.
Discussion
Broadband availability was associated with greater telemedicine use, but only in fully rural counties. The FCC’s Connect America Fund has awarded billions of dollars in subsidies to expand broadband, but most of that funding is in counties where we did not observe an association between broadband availability and telemedicine use. More targeted funding to fully rural counties, where wired broadband may be a critical barrier, could help to alleviate disparities in access to health specialists.
Our analysis was limited to wired broadband availability and may not represent all connectivity options available and our measure of telemedicine only captures when health care professionals bill for telemedicine visits.
References
- 1.Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009;60(10):1323-1328. doi:10.1176/ps.2009.60.10.1323 [DOI] [PubMed] [Google Scholar]
- 2.Mehrotra A, Huskamp HA, Souza J, et al. . Rapid growth in mental health telemedicine use among rural Medicare beneficiaries, wide variation across states. Health Aff (Millwood). 2017;36(5):909-917. doi:10.1377/hlthaff.2016.1461 [DOI] [PubMed] [Google Scholar]
- 3.Federal Communications Commission. Connect America Fund phase II auction (auction 903). https://www.fcc.gov/auction/903. Updated June 10, 2019. Accessed June 25, 2019.
- 4.Federal Communications Commission. Fixed broadband deployment data from FCC form 477. https://www.fcc.gov/general/broadband-deployment-data-fcc-form-477. Updated May 2, 2019. Accessed September 28, 2018.
- 5.Federal Communications Commission. 2018 Broadband deployment report. https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2018-broadband-deployment-report. Updated February 5, 2018. Accessed March 1, 2019.
- 6.United States Department of Agriculture Economic Research Service. Rural-urban continuum curves. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/. Updated October 12, 2016. Accessed September 28, 2018.