The omicron variant of SARS-CoV-2 (PANGO B.1.1.529) spread rapidly across the world, out-competing former variants soon after it was first detected in November, 2021. According to the Our World in Data COVID-19 database, In Europe, the number of confirmed cases reported between December, 2021, and March, 2022 (omicron period) has exceeded all previously reported cases. Omicron appears to cause less severe acute illness than previous variants, at least in vaccinated populations. However, the potential for large numbers of people to experience long-term symptoms is a major concern, and health and workforce planners need information urgently to appropriately scale resource allocation.
In this case-control observational study, we set out to identify the relative odds of long-COVID (defined following the National Institute for Health and Care Excellence guidelines as having new or ongoing symptoms 4 weeks or more after the start of acute COVID-19) in the UK during the omicron period compared with the delta period. We used self-reported data from the COVID Symptom Study app1 (King's College London Research Ethics Management Application System number 18210, reference LRS-19/20-18210). Data were extracted and pre-processed using ExeTera13 (version 0.5.5).
The inclusion criteria in both periods were a positive real-time PCR or lateral flow antigen test for SARS-CoV-2 after vaccination, at least one log per week in the app for at least 28 days after testing positive,2 and no previous SARS-CoV-2 infections before vaccination.
We identified 56 003 UK adults first testing positive between Dec 20, 2021, and March 9, 2022, who satisfied the inclusion criteria. These cases are hereafter referred to as omicron cases as more than 70% of UK cases were estimated to be attributable to the omicron variant during that time. Using identical selection criteria, we identified 41 361 UK adult cases first testing positive between June 1, 2021, and Nov 27, 2021, referred to as delta cases as more than 70% of cases were attributable to the delta variant. Both symptomatic and asymptomatic infections were considered, and, for the omicron period, we included only participants testing positive before Feb 10, 2022, to ensure all participants had at least 28 days for symptom reporting after testing positive.
In both periods, female participation was higher than male participation (55% for omicron and 59% for delta cases). Delta and omicron cases had similar age (mean age 53 years) and prevalence of comorbidities (around 19%). Considering the local area Index of Multiple Deprivation (IMD), a score ranging from 1 (most deprived) to 10 (least deprived) estimating relative locality deprivation, omicron cases were distributed in areas of slightly lower deprivation than delta cases (16·7% vs 17·5% for IMD 1–3). To assess the association between long COVID (outcome) and the infection period (exposure), we applied a univariate logistic regression model adjusted by sex, IMD, age, the presence of comorbidities, vaccination status (one, two, or three doses), and body-mass index, all of which are related to the risk of long COVID.3 We stratified the analysis according to the time elapsed between infection and most recent vaccination considering three groups, 3 months, 3–6 months, and more than 6 months, to allow for potential waning of immunity from vaccination.
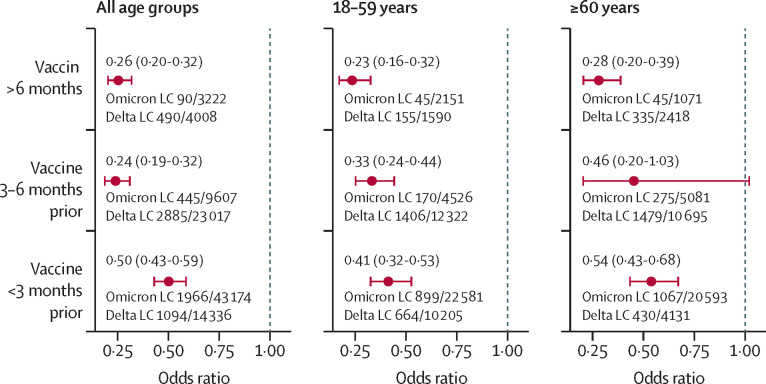
Among omicron cases, 2501 (4·5%) of 56 003 people experienced long COVID and, among delta cases, 4469 (10·8%) of 41 361 people experienced long COVID. Omicron cases were less likely to experience long COVID for all vaccine timings, with an odds ratio ranging from 0·24 (0·20–0·32) to 0·50 (0·43–0·59). These results were also confirmed when the analysis was stratified by age group (figure ).
Figure.
Odds ratio of long COVID (LC) adjusted by age, sex, body-mass index, Index of Multiple Deprivation, presence of comorbidities, and vaccination status
Omicron long COVID and delta long COVID indicate, for each stratum, the number of users with long COVID over the total number of users of that stratum.
We believe this is the first peer-reviewed study to report on long COVID risk associated with infection by the omicron variant, highlighting that health surveillance using smartphone apps can produce rapid insights, which we have consistently shown are accurate and subsequently replicated.1 A major strength of our study in relation to long COVID is the prospective symptom logging of a wide range of symptoms. Limitations of the self-reported data include no direct testing of infectious variants (here assumed from national data) and no objective measures of illness duration. The samples, although not fully generalisable to the UK population on account of sex and socioeconomic bias, were similar in both periods, allowing comparison. We had insufficient data to estimate the odds of long COVID in unvaccinated individuals and did not estimate effects in children. Finally, to enable swift reporting, the period of assessment of omicron cases was slightly shorter than for the delta variant, and assessment of longer durations of long COVID (eg, >12 weeks) was not possible.
Overall, we found a reduction in odds of long COVID with the omicron variant versus the delta variant of 0·24–0·50 depending on age and time since vaccination. However, the absolute number of people experiencing long COVID at a given time depends on the shape and amplitude of the pandemic curve. For example, given the high numbers of people infected with omicron in the UK from December, 2021, to February, 2022, our data are consistent with the UK Office for National Statistics, who estimated that the numbers of people experiencing long COVID actually increased from 1·3 million in January, 2022, to 1·7 million in March, 2022.4 Considering the UK omicron peak of more than 350 000 new symptomatic COVID-19 cases per day estimated on March 26, 2022, by the ZOE app model and 4% of cases being long COVID, future numbers with long COVID will inevitably rise.
For Our World In Data COVID-19 data see https://ourworldindata.org/coronavirus
Acknowledgments
SO and CJS contributed equally. TDS is a co-founder and shareholder of ZOE. JCP is an employee at ZOE. SO and CS have consulted for ZOE. MA declares no competing interests. This work is supported by the UK Department of Health via the National Institute for Health Research comprehensive Biomedical Research Centre award to Guy's & St Thomas’ and King's College Hospital NHS Foundation Trusts and King's College London, and via a grant to ZOE from the UK Health Security Agency. This work is also supported by the Chronic Disease Research Foundation and the Wellcome Engineering and Physical Sciences Research Council Centre for Medical Engineering at King's College London.
References
- 1.Varsavsky T, Graham MS, Canas LS, et al. Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study. Lancet Public Health. 2021;6:e21–e29. doi: 10.1016/S2468-2667(20)30269-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22:43–55. doi: 10.1016/S1473-3099(21)00460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office for National Statistics Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK. 3 March 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/3march2022